Yes! You can use AI to fill out Horizon Blue Cross Blue Shield of New Jersey Applied Behavior Analysis Supplemental Information Form
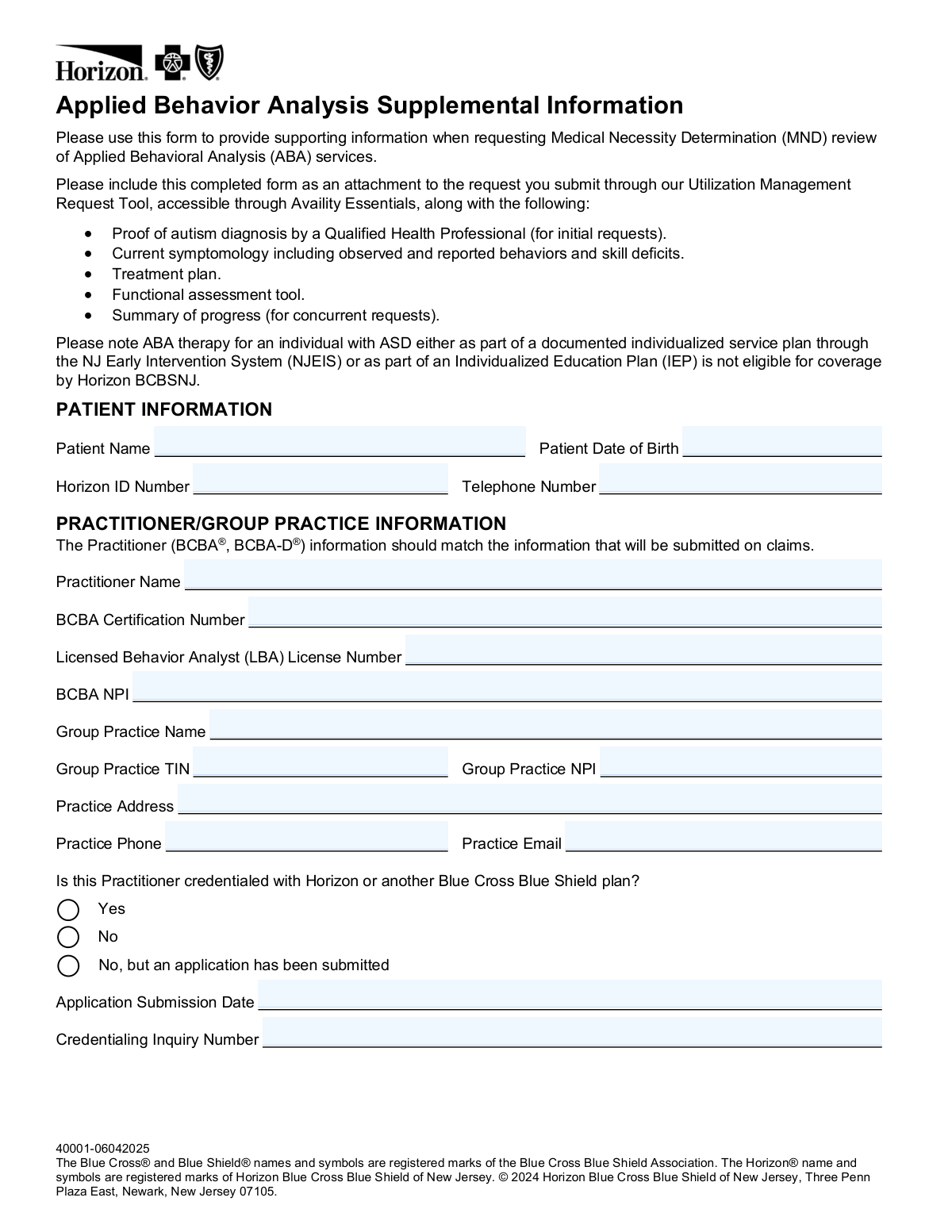
The Horizon Blue Cross Blue Shield of New Jersey Applied Behavior Analysis Supplemental Information Form is a clinical documentation form required when requesting Medical Necessity Determination (MND) review for ABA therapy services for members diagnosed with Autism Spectrum Disorder (ASD). It captures patient demographics, BCBA practitioner credentials, requested ABA service codes and units, program settings, autism severity levels, treatment progress, and care management needs. The form must be submitted as an attachment through Horizon's Utilization Management Request Tool via Availity Essentials, along with supporting documents such as proof of autism diagnosis and a treatment plan. Today, this form can be filled out quickly and accurately using AI-powered services like Instafill.ai, which can also convert non-fillable PDF versions into interactive fillable forms.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out Horizon BCBSNJ ABA Supplemental Information Form using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Horizon Blue Cross Blue Shield of New Jersey Applied Behavior Analysis Supplemental Information Form |
| Number of pages: | 5 |
| Language: | English |
Instafill Demo: filling out a legal form in seconds
How to Fill Out Horizon BCBSNJ ABA Supplemental Information Form Online for Free in 2026
Are you looking to fill out a HORIZON BCBSNJ ABA SUPPLEMENTAL INFORMATION FORM form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your HORIZON BCBSNJ ABA SUPPLEMENTAL INFORMATION FORM form in just 37 seconds or less.
Follow these steps to fill out your HORIZON BCBSNJ ABA SUPPLEMENTAL INFORMATION FORM form online using Instafill.ai:
- 1 Navigate to Instafill.ai and upload the Horizon BCBSNJ ABA Supplemental Information Form PDF, or select it from the available form library to begin filling it out online.
- 2 Enter the patient information section, including the patient's full name, date of birth, Horizon ID number, and telephone number.
- 3 Complete the Practitioner/Group Practice Information section with the BCBA's name, certification number, LBA license number, NPI, group practice name, TIN, group practice NPI, practice address, phone, email, and credentialing status with Horizon or another BCBS plan.
- 4 Select the type of service being requested (Initial Assessment, Initial Treatment, or Concurrent Review), enter the requested start date, and specify the program setting(s) and hours per week for each applicable setting.
- 5 Fill in the Services Requested section by entering the units requested (and units used from the previous authorization period for concurrent reviews) for each applicable ABA service code, including assessment, treatment planning, direct therapy, group treatment, and family guidance services.
- 6 Complete the Patient Condition and Progress section by selecting DSM-V autism severity levels for social communication and restrictive/repetitive behaviors, indicating any IDD diagnosis, percentage of goals mastered, treatment domains addressed, and any treatment barriers or standardized/curriculum assessment results.
- 7 Review all sections for accuracy, add any additional clinical notes, indicate whether health plan care management services would be helpful, and then submit the completed form as an attachment through Horizon's Utilization Management Request Tool via Availity Essentials along with all required supporting documentation.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable Horizon BCBSNJ ABA Supplemental Information Form Form?
Speed
Complete your Horizon BCBSNJ ABA Supplemental Information Form in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 Horizon BCBSNJ ABA Supplemental Information Form form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form Horizon BCBSNJ ABA Supplemental Information Form
This form is used to provide supporting clinical information when requesting a Medical Necessity Determination (MND) review for Applied Behavioral Analysis (ABA) services from Horizon Blue Cross Blue Shield of New Jersey. It must be submitted alongside other required documents through the Utilization Management Request Tool on Availity Essentials.
This form must be completed by a Board Certified Behavior Analyst (BCBA® or BCBA-D®) or their group practice when requesting authorization for ABA therapy services for a patient with Autism Spectrum Disorder (ASD). The practitioner information entered must match what will be submitted on claims.
Along with the completed form, you must include: proof of autism diagnosis by a Qualified Health Professional (for initial requests), current symptomology including observed and reported behaviors and skill deficits, a treatment plan, a functional assessment tool, and a summary of progress (for concurrent requests only).
You must submit this completed form as an attachment through the Utilization Management Request Tool, which is accessible via Availity Essentials. The form should not be submitted on its own — it must accompany your full authorization request.
No. ABA therapy for an individual with ASD that is part of a documented individualized service plan through the NJ Early Intervention System (NJEIS) or part of an Individualized Education Plan (IEP) is not eligible for coverage by Horizon BCBSNJ.
This form supports three types of requests: Initial Assessment, Initial Treatment, and Concurrent Review. You must select the appropriate service type and provide the relevant details, including requested start date, program settings, hours per week, and specific service codes with units requested.
You must provide a written explanation in the designated section on page 3 of the form. If more space is needed, you may include a separate sheet. This explanation is required for concurrent review requests whenever requested units exceeded used units for any service.
The practitioner must be a BCBA® or BCBA-D® and must provide their BCBA Certification Number, Licensed Behavior Analyst (LBA) License Number, and BCBA NPI. The practitioner must also indicate whether they are credentialed with Horizon or another Blue Cross Blue Shield plan.
If the practitioner is not credentialed but has submitted an application, you should select 'No, but an application has been submitted' and provide the Application Submission Date and Credentialing Inquiry Number in the designated fields.
Autism symptom severity is reported using DSM-5 classifications separately for Social Communication/Interaction and Restrictive/Repetitive Behaviors. Each category is rated as Level 1 (requiring support), Level 2 (requiring substantial support), Level 3 (requiring very substantial support), or Unknown.
For concurrent review, you must report the percentage of proposed goals mastered during the last authorization period (in ranges: 100%-76%, 75%-51%, 50%-26%, or 25% or less), any treatment barriers encountered, caregiver participation in treatment, and results from any standardized or curriculum assessments administered in the past year.
Yes, AI-powered services like Instafill.ai can help you accurately auto-fill form fields, saving time and reducing errors. If the PDF version of this form is not fillable, Instafill.ai can also convert flat, non-fillable PDFs into interactive fillable forms so you can complete them digitally.
Simply upload the ABA Supplemental Information form PDF to Instafill.ai, and the AI will guide you through completing each field accurately. Once filled out, you can download the completed form and attach it to your Utilization Management Request through Availity Essentials.
The form covers multiple CPT/HCPCS codes including 97151, 97152, 0362T (assessment services), H0032 (treatment planning), 97153, 97154, 97155, 0373T (direct ABA therapy), 97158 (group treatment), and 97156, 97157 (family training). Most services are measured in 15-minute increments, and you must specify hours per week, days per week, and total units requested.
The form allows practitioners to indicate whether health plan care management services would be helpful for the member, including care coordination, addressing comorbid medical conditions, homelessness, living situation, food insecurity, transportation, health literacy, referrals for community resources, transition to community services, or other treatment barriers.
Compliance Horizon BCBSNJ ABA Supplemental Information Form
Validation Checks by Instafill.ai
1
Patient Date of Birth Format and Validity
Validates that the Patient Date of Birth is entered in a standard date format (MM/DD/YYYY) and represents a logically valid date (e.g., not a future date, not more than 120 years in the past). This field is critical for correctly identifying the member in Horizon's system and ensuring the authorization is tied to the correct individual. If the date is missing, improperly formatted, or logically invalid, the request cannot be processed and may be rejected or delayed.
2
Horizon ID Number Format Validation
Ensures the Horizon ID Number is present and conforms to Horizon BCBSNJ's expected member ID format, typically a combination of letters and numbers of a specific length. An incorrect or missing Horizon ID will prevent the system from locating the member's eligibility and benefits, causing the MND request to fail. This field must exactly match the ID on the member's insurance card to avoid misidentification.
3
BCBA Certification Number Format and Presence
Validates that the BCBA Certification Number is provided and follows the expected alphanumeric format issued by the Behavior Analyst Certification Board (BACB). ABA services must be directed by a credentialed BCBA or BCBA-D, and this number is used to verify the practitioner's qualifications. If this field is missing or incorrectly formatted, the request may be denied as the practitioner's credentials cannot be confirmed.
4
NPI Number Format Validation for Practitioner and Group Practice
Checks that both the BCBA NPI and Group Practice NPI fields contain valid 10-digit National Provider Identifier numbers, as required by HIPAA standards. NPIs are used to identify healthcare providers on claims, and the form explicitly states that practitioner information must match what will be submitted on claims. An invalid or mismatched NPI will cause a discrepancy between the authorization request and subsequent claims submissions, leading to claim denials.
5
Group Practice Tax Identification Number (TIN) Format Validation
Ensures the Group Practice TIN is entered in the correct format (XX-XXXXXXX, a 9-digit Employer Identification Number). The TIN is required for billing and reimbursement purposes and must match the information on file with Horizon BCBSNJ. A missing or incorrectly formatted TIN will prevent proper claims processing and could result in payment delays or denials.
6
Credentialing Status Conditional Field Completeness
Validates that when the practitioner selects 'No, but an application has been submitted' for the credentialing question, both the Application Submission Date and Credentialing Inquiry Number fields are populated. These fields are conditionally required to allow Horizon to track the pending credentialing application and assess the request appropriately. If the credentialing option is selected but the supporting fields are left blank, the submission is incomplete and cannot be properly evaluated.
7
Service Type Selection Requirement
Ensures that exactly one service type is selected from the options: Initial Assessment, Initial Treatment, or Concurrent Review. This selection determines which sections of the form are applicable and what supporting documentation is required (e.g., proof of autism diagnosis for initial requests, summary of progress for concurrent reviews). If no service type is selected, the form is incomplete and the appropriate review pathway cannot be determined.
8
Concurrent Review Fields Populated Only for Concurrent Requests
Validates that 'Units Used from Previous Authorization Period' fields are only completed when 'Concurrent Review' is selected as the service type, and that these fields are not left blank when a concurrent review is requested. Submitting prior-period usage data for an initial request is illogical and may indicate a form error, while omitting this data for a concurrent review prevents Horizon from evaluating utilization patterns. This logical consistency check ensures the form data aligns with the selected review type.
9
Units Requested Greater Than Units Used Explanation Requirement
Checks that when any 'Units Requested' value for a concurrent review exceeds the corresponding 'Units Used from Previous Authorization Period' value, the explanation field on page 3 is completed with a non-blank, substantive response. The form explicitly requires justification for under-utilization relative to the new request, as this discrepancy may indicate a change in the member's needs or treatment plan. Failure to provide this explanation when required will result in an incomplete submission that cannot be reviewed.
10
Program Setting Hours Per Week Consistency with Units Requested
Validates that the total hours per week indicated across all program settings (Member's Home, Facility/Clinic, Other) are logically consistent with the total units requested for direct therapy services, given that units are measured in 15-minute increments. For example, if 40 hours per week are listed across settings, the total units requested for direct services should approximate 160 units per week. Significant discrepancies between setting hours and requested units may indicate data entry errors that would affect authorization accuracy.
11
H0032 Treatment Planning Units Cap Validation
Ensures that the units requested for H0032 (Treatment Planning by BCBA) do not exceed the maximum allowable limit of 4 units per treatment week, as explicitly stated in the form instructions. Submitting a request that exceeds this cap will result in automatic denial of the excess units and may flag the entire request for additional scrutiny. The validation should calculate the total units requested against the number of treatment weeks in the authorization period to confirm compliance.
12
DSM-V Autism Severity Classification Selection Requirement
Validates that exactly one severity level is selected for each of the two DSM-V autism severity classification categories: Social Communication/Interaction and Restrictive/Repetitive Behaviors. These classifications are required to establish medical necessity and determine the appropriate level of ABA services. If either classification is left unselected, the clinical picture is incomplete and the MND review cannot be properly conducted.
13
Percent of Goals Mastered Field Required for Concurrent Reviews
Ensures that the 'Percent of proposed goals mastered during last authorization period' field is completed when the request type is Concurrent Review, as this metric is a key indicator of treatment progress and effectiveness. This information is used by Horizon to assess whether continued ABA services at the requested level are medically necessary. If this field is blank for a concurrent review, the submission lacks critical clinical data required for the review determination.
14
Treatment Barriers Field Completeness Validation
Validates that the treatment barriers field contains either a substantive description of identified barriers and the plan to address them, or explicitly states 'N/A' as instructed. A blank field is not acceptable, as it is ambiguous whether barriers were not identified or the question was simply overlooked. This information is important for care management planning and for understanding factors that may have affected the member's participation in treatment during the prior authorization period.
15
Standardized and Curriculum Assessment Fields Completeness
Checks that both the standardized assessment field and the curriculum assessment field contain either a valid entry (instrument name, date administered, and score) or explicitly state 'N/A' as instructed, and that any assessment date provided falls within the last 12 months. Assessments older than one year may not accurately reflect the member's current functional level and could undermine the clinical justification for services. Blank fields or entries with missing components (e.g., score without instrument name) are flagged as incomplete.
16
Practice Email Format Validation
Ensures the Practice Email field, if completed, contains a properly formatted email address following the standard pattern (e.g., [email protected]), including a local part, an '@' symbol, and a valid domain. An incorrectly formatted email address will prevent Horizon from communicating authorization decisions or requesting additional information from the practice. While the field may not be strictly required, any value entered must be a valid, reachable email address to facilitate timely communication.
Common Mistakes in Completing Horizon BCBSNJ ABA Supplemental Information Form
The form explicitly states that the Practitioner (BCBA®, BCBA-D®) information must match what will be submitted on claims, yet providers frequently enter slightly different names, NPIs, or addresses than what is on file with Horizon. This mismatch can cause claim denials or delays in the MND review process. Always verify that the practitioner name, BCBA NPI, and Group Practice NPI on this form exactly match the credentialing and billing records on file. Tools like Instafill.ai can help auto-populate and validate practitioner data consistently across submissions.
Multiple service codes (e.g., 97151, 97152, H0032, 97153, 97154, 97155, 97156, 97157, 97158, 0373T) are billed in 15-minute increments, meaning 1 hour equals 4 units. Providers commonly enter hours instead of units in the 'Units Requested' fields, resulting in a significant underestimate or overestimate of the services being requested. This can lead to authorization for far fewer or more services than clinically needed. Always convert hours to units (multiply hours by 4) before entering values, and double-check each service code's unit definition as stated in the form.
When submitting a Concurrent Review request, providers are required to fill in both 'Units Requested' and 'Units Used from Previous Authorization Period' for each applicable service code. Many providers leave the 'Units Used' field blank, either because they forget or assume it is optional. Omitting this data can result in the request being returned or denied due to incomplete information. Carefully track utilization data from the previous authorization period and have it ready before completing the form.
The form requires a written explanation whenever the units requested for the upcoming period are greater than the units actually used during the previous authorization period. Providers frequently overlook this requirement and leave the explanation section on page 3 blank, which raises red flags for reviewers and can result in denial or requests for additional information. Always review the units requested versus units used for every service code and provide a clear, clinically justified explanation for any discrepancy in the designated space.
For initial requests, the form requires proof of autism diagnosis by a Qualified Health Professional to be submitted as an attachment alongside the completed form. Providers frequently submit the form through the Utilization Management Request Tool without including this documentation, causing delays or outright denial of the MND review. Ensure that a copy of the qualifying autism diagnosis documentation is prepared and attached every time an Initial Assessment or Initial Treatment request is submitted.
The form clearly states that ABA therapy provided as part of a documented individualized service plan through the NJ Early Intervention System (NJEIS) or as part of an Individualized Education Plan (IEP) is not eligible for coverage by Horizon BCBSNJ. Providers sometimes submit requests for services that are already being funded through these programs, leading to automatic denial. Before submitting, confirm that the requested ABA services are not duplicated under an active NJEIS plan or IEP, and document this clearly in the clinical notes if relevant.
Providers must indicate whether the practitioner is credentialed with Horizon or another Blue Cross Blue Shield plan, and if an application has been submitted, they must provide both the Application Submission Date and the Credentialing Inquiry Number. Many providers select 'No, but an application has been submitted' without filling in these two required follow-up fields, leaving the reviewer without the information needed to verify credentialing status. Always have the application submission date and credentialing inquiry number on hand before completing this section.
The form requires separate DSM-5 autism severity classifications for two distinct domains: Social Communication/Interaction AND Restrictive/Repetitive Behaviors. Providers frequently complete only one of the two severity sections, either because they misread the form or assume one answer covers both domains. Leaving one domain blank results in an incomplete clinical picture and may delay the review. Carefully read both sections and select the appropriate severity level (Level 1, 2, or 3, or 'Unknown') for each domain independently.
The form explicitly instructs providers to write 'N/A' in the standardized assessment and curriculum assessment fields if no such assessments have been administered or used. Many providers simply leave these fields blank, which can be interpreted as an oversight or incomplete submission rather than a deliberate indication that no assessment was conducted. Always enter 'N/A' as instructed when the field does not apply, and include the instrument name, date administered, and score when an assessment has been completed within the required timeframe.
The form requires providers to either describe any treatment barriers identified over the past 6-month period along with a plan to address them, or explicitly write 'N/A' if no barriers were identified. Providers often skip this field entirely, particularly when they believe there are no barriers to report. A blank field can signal an incomplete form to reviewers and may slow down the authorization process. Always address this field with either a substantive explanation or 'N/A' as directed.
The form requires two separate NPIs: the individual BCBA NPI and the Group Practice NPI. Providers frequently enter the same NPI in both fields, or swap the individual and group NPIs, which causes mismatches during claims processing and credentialing verification. The individual BCBA NPI is a Type 1 NPI assigned to the practitioner, while the Group Practice NPI is a Type 2 NPI assigned to the organization. Verify both NPIs independently before entering them, and consider using a tool like Instafill.ai to auto-validate NPI formats and prevent transposition errors.
The form includes patient name and Horizon ID header fields at the top of pages 2, 3, 4, and 5, which must be completed on each page to ensure proper identification if pages become separated during processing. Providers commonly fill in this information only on the first page and leave subsequent page headers blank. If pages are separated or scanned individually, missing identifiers can result in lost or misrouted documentation. Make it a standard practice to complete the patient name and Horizon ID fields at the top of every page before submitting.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out Horizon BCBSNJ ABA Supplemental Information Form with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills horizon-blue-cross-blue-shield-of-new-jersey-applied-behavior-analysis-supplemental-information-form forms, ensuring each field is accurate.