Fill out Form BHVH, Outpatient Behavioral Health – ABA Treatment Request with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills OUTPATIENT-BEHAVIORAL-HEALTH-BH-ABA-ASSESSMENT-PRECERT forms, ensuring each field is accurate.
#1 AI PDF Filling Software of 2026
3 out of 4 customers say they prepare their BHVH forms in 37 seconds or less
Secure platform for your PDF forms and personal information
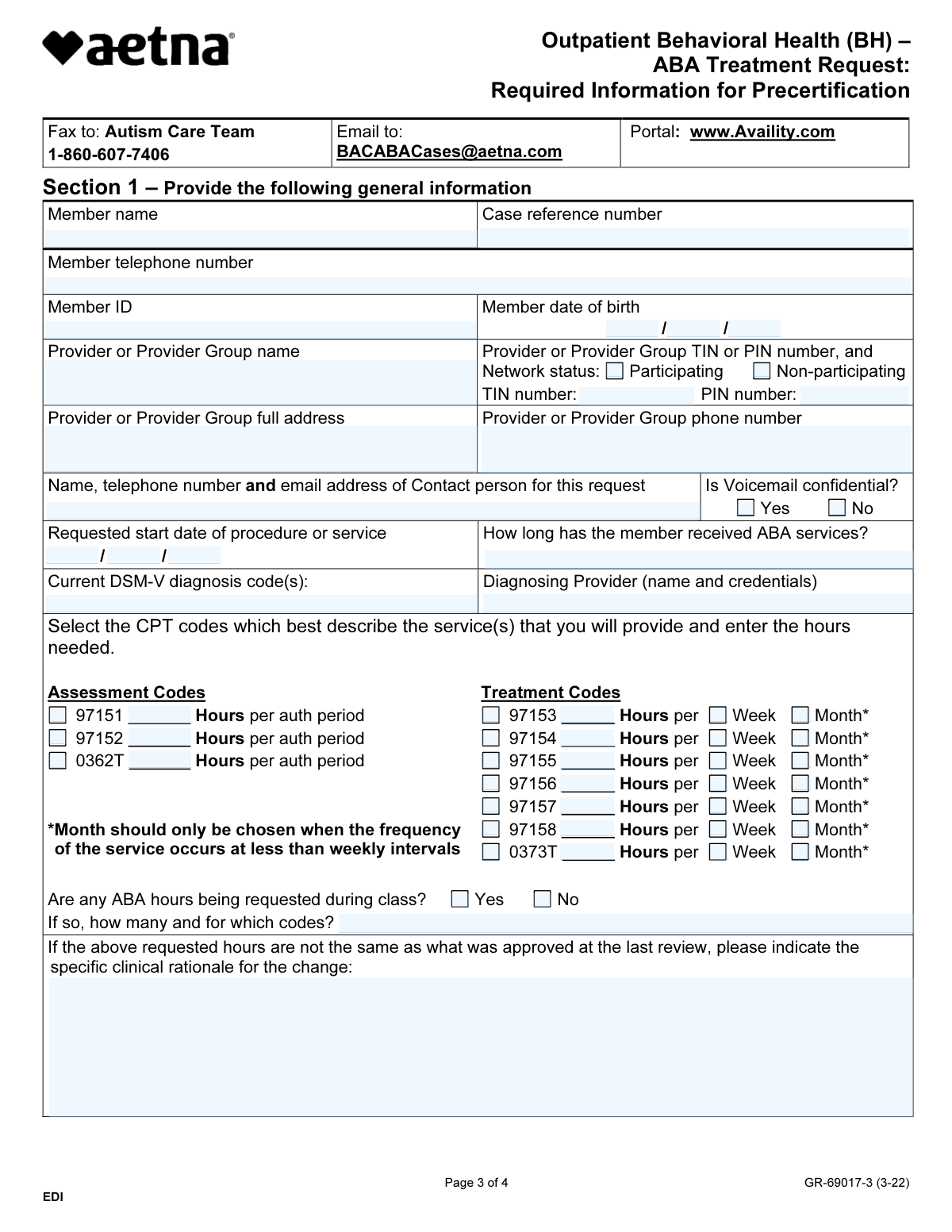
| Form name: | Form BHVH, Outpatient Behavioral Health – ABA Treatment Request |
| Number of pages: | 4 |
Instafill Demo: filling out a legal form in seconds
Compliance BHVH
Validation Checks by Instafill.ai
1
Member Information Validation
This validation check confirms that the member's name, case reference number, telephone number, ID, and date of birth are accurately filled in. It ensures that all required personal information is complete and correctly formatted, which is crucial for the processing of the treatment request. By verifying these details, the system helps to prevent any potential delays or issues in the approval process. This check is essential for maintaining accurate records and ensuring that the request is associated with the correct member.
2
Provider Information Validation
This validation check ensures that the provider or provider group name, TIN or PIN number, and participation status (participating or non-participating) are clearly indicated. It verifies that the necessary provider details are present, which is vital for determining eligibility and reimbursement for services rendered. By confirming this information, the system helps to streamline the authorization process and ensures compliance with regulatory requirements. This check is important for establishing the legitimacy of the provider involved in the treatment request.
3
Provider Contact Information Validation
This validation check verifies that the full address and phone number of the provider or provider group are provided. It ensures that the contact information is complete and accurate, which is essential for communication regarding the treatment request. By checking this information, the system helps to facilitate timely follow-ups and clarifications if needed. This check is crucial for maintaining effective communication between all parties involved in the treatment process.
4
Contact Person Information Validation
This validation check checks that the contact person's name, telephone number, and email address for the request are included, along with the indication of whether voicemail is confidential. It ensures that there is a designated point of contact for any inquiries or updates related to the treatment request. By verifying this information, the system helps to enhance communication efficiency and confidentiality. This check is important for ensuring that sensitive information is handled appropriately.
5
Requested Start Date Validation
This validation check ensures that the requested start date for the procedure or service is specified. It verifies that the treatment timeline is clearly outlined, which is essential for scheduling and resource allocation. By confirming the start date, the system helps to align the treatment plan with the member's needs and availability. This check is crucial for ensuring that the treatment process can commence without unnecessary delays.
6
Confirms that the duration for which the member has been receiving ABA services is documented.
This validation check ensures that the form accurately reflects the length of time the member has been engaged in ABA services. It verifies that the documentation is complete and provides a clear timeline of service delivery. By confirming this information, the software helps to maintain continuity of care and supports the treatment planning process. This check is crucial for assessing the member's progress and determining the appropriateness of ongoing services.
7
Verifies that the current DSM-V diagnosis code(s) and the name and credentials of the diagnosing provider are included.
This validation check verifies that the form includes the necessary DSM-V diagnosis code(s) relevant to the member's condition. It ensures that the diagnosing provider's name and credentials are accurately documented, which is essential for establishing the legitimacy of the diagnosis. By confirming this information, the software helps to uphold the standards of clinical practice and ensures that the treatment request is based on a valid diagnosis. This check is vital for compliance with insurance requirements and for facilitating appropriate treatment interventions.
8
Ensures that the appropriate CPT codes are selected and the required hours for each code are entered.
This validation check ensures that the form includes the correct CPT codes that correspond to the services being requested. It verifies that the required number of hours for each selected code is accurately entered, which is essential for proper billing and reimbursement. By confirming this information, the software helps to prevent errors that could lead to claim denials or delays in payment. This check is crucial for ensuring that the treatment request aligns with coding guidelines and reflects the services provided.
9
Checks if any ABA hours requested during class are indicated, along with the number of hours and codes if applicable.
This validation check checks whether the form specifies any ABA hours that are requested to be provided during class settings. It ensures that the number of hours and corresponding codes are clearly indicated, which is important for understanding the context of service delivery. By verifying this information, the software helps to ensure that the treatment plan is comprehensive and considers all aspects of the member's needs. This check is essential for facilitating effective communication between providers and ensuring that all services are accounted for.
10
Verifies that a clinical rationale is provided if the requested hours differ from the last review.
This validation check verifies that a clinical rationale is included in the form if the requested hours for ABA services differ from those established in the last review. It ensures that there is a clear justification for any changes in service hours, which is critical for maintaining transparency and accountability in treatment planning. By confirming this information, the software helps to support clinical decision-making and ensures that the treatment request is based on sound clinical reasoning. This check is important for fostering trust between providers and payers, as well as for ensuring that the member's needs are adequately addressed.
11
Confirms that the supervising or directing individual for ABA services is identified
This validation check ensures that the supervising or directing individual for ABA services is clearly identified on the form. It verifies that their name, credentials, and phone number are provided, which is crucial for accountability and communication. Additionally, it confirms that voicemail confidentiality is indicated, safeguarding the privacy of the individual. This thorough identification process is essential for maintaining the integrity of the treatment request.
12
Verifies that essential elements such as a diagnosis of Autism Spectrum Disorder are met
This check verifies that all essential elements required for the ABA treatment request are present and accurately documented. It ensures that a diagnosis of Autism Spectrum Disorder is included, which is a fundamental criterion for the treatment. Furthermore, it confirms that identifiable target behaviors, parental participation, and a time-limited treatment plan are also specified. This comprehensive verification process is vital for the appropriateness and effectiveness of the requested services.
13
Ensures that any additional services the member is receiving are checked and confirmed
This validation check ensures that any additional services the member is currently receiving are properly checked and confirmed on the form. It verifies that the information is complete and accurately reflects the member's overall treatment plan. This is important for coordinating care and avoiding service duplication. By confirming these additional services, the check supports a holistic approach to the member's behavioral health needs.
14
Checks that supporting documentation is included with the request
This validation check verifies that all necessary supporting documentation is included with the ABA treatment request. It ensures that standardized assessment results and individualized treatment plans are attached, which are critical for substantiating the request. This thorough documentation check is essential for facilitating a comprehensive review of the treatment needs. By confirming the inclusion of these documents, the check enhances the likelihood of a timely and informed decision regarding the request.
15
Ensures that the form is signed by the appropriate individual
This validation check ensures that the form is signed by the appropriate individual, confirming who completed it and their title. It verifies that the signature is present, which is essential for accountability and authenticity of the request. This check is important for establishing a clear line of responsibility for the information provided. By confirming the signature, the check reinforces the integrity of the submission process.
Common Mistakes in Completing BHVH
Providing an incorrect member's name or case reference number can lead to delays in processing the treatment request. It is essential to double-check the member's information against official documents to ensure accuracy. To avoid this mistake, verify the details with the member or their guardian before submission. Additionally, cross-reference the case reference number with the relevant records to confirm it is correct.
Omitting or incorrectly entering the telephone number or ID can hinder communication and lead to processing issues. Ensure that all contact information is accurate and up-to-date by reviewing it carefully before submission. It is advisable to include a secondary contact number if available, to facilitate easier communication. Always confirm the format of the ID number required to avoid any discrepancies.
Failing to include the provider's Tax Identification Number (TIN) or Provider Identification Number (PIN) can result in the request being rejected. This information is crucial for verifying the provider's credentials and ensuring proper billing. To prevent this error, make it a habit to check that all required identification numbers are included in the form. Additionally, consult the provider's records to ensure the numbers are accurate and current.
Neglecting to indicate the provider's participation status can create confusion regarding coverage and reimbursement. It is important to clearly state whether the provider is in-network or out-of-network to avoid misunderstandings. To mitigate this issue, familiarize yourself with the provider's network status and ensure it is clearly marked on the form. Regularly updating this information can also help maintain clarity in future requests.
Submitting an incomplete provider address or phone number can lead to difficulties in contacting the provider for follow-up or clarification. Ensure that all contact details are fully filled out, including street address, city, state, and zip code. To avoid this mistake, use a checklist to confirm that all sections of the address are complete before submission. Additionally, consider including an email address for further communication options.
Omitting the contact person's name or email address can lead to delays in processing the treatment request. It is essential to provide complete contact information to ensure that the relevant parties can communicate effectively. To avoid this mistake, double-check that all required fields are filled out completely, including the contact person's details. Additionally, consider providing an alternative contact method in case of any issues.
Not indicating whether voicemail messages are confidential can create privacy concerns and hinder communication. It is crucial to clarify this aspect to ensure that sensitive information is handled appropriately. To prevent this oversight, take a moment to review the voicemail confidentiality section and provide a clear indication of your preferences. This will help maintain confidentiality and ensure that communication remains secure.
Failing to include the requested start date for services can result in delays in the initiation of treatment. It is important to specify when services are expected to begin to facilitate timely scheduling and resource allocation. To avoid this mistake, carefully review the form and ensure that the start date is clearly indicated. Providing this information upfront will help streamline the process and ensure that services commence as planned.
Leaving out the duration of ABA services previously received can lead to misunderstandings regarding the patient's treatment history. This information is vital for assessing the patient's needs and planning future services. To avoid this error, make sure to include the total duration of any prior ABA services in the designated section of the form. This will provide a clearer picture of the patient's background and assist in making informed decisions about their care.
Not providing the DSM-V diagnosis code(s) can hinder the approval process for treatment requests. Accurate diagnosis codes are essential for insurance purposes and to ensure that the treatment plan aligns with the patient's needs. To prevent this mistake, verify that you have the correct diagnosis codes before submitting the form. Consulting with a healthcare professional or referring to the DSM-V can help ensure that all necessary codes are included.
Omitting the diagnosing provider's name and credentials can lead to delays in processing the treatment request. It is essential to ensure that this information is accurately filled out to establish the legitimacy of the diagnosis. To avoid this mistake, double-check that the provider's full name, title, and credentials are clearly stated on the form. Additionally, confirm that the information matches what is on file with the relevant health authorities.
Selecting incorrect CPT codes can result in claim denials or delays in authorization for services. It is crucial to review the list of applicable CPT codes and ensure that the codes selected accurately reflect the services being requested. To prevent this error, familiarize yourself with the coding guidelines and consult with a coding specialist if necessary. Always verify that the codes align with the specific treatment being provided.
Failing to specify the required hours for each CPT code can lead to incomplete requests and subsequent delays in service approval. Each CPT code must have the corresponding number of hours clearly indicated to ensure proper authorization. To avoid this mistake, carefully review the requirements for each code and ensure that the hours are accurately documented. It may be helpful to create a checklist to confirm that all necessary information is included before submission.
Not indicating the ABA hours during class can result in misunderstandings regarding the treatment plan and its implementation. It is important to provide a clear account of the hours dedicated to ABA therapy during class sessions to ensure comprehensive treatment coverage. To mitigate this issue, maintain detailed records of therapy hours and include them in the request. Regularly updating this information can help ensure accuracy and completeness.
Neglecting to provide a clinical rationale for any changes in hours can lead to questions about the necessity of the adjustments. A well-documented rationale is essential for justifying the requested changes and ensuring that they are understood by the reviewing authority. To avoid this mistake, always include a clear and concise explanation for any modifications in hours, supported by clinical evidence. This practice not only strengthens the request but also enhances communication with the reviewing body.
Omitting the supervisor's name, credentials, or phone number can lead to delays in processing the treatment request. It is essential to provide complete and accurate contact information to ensure that communication can occur without issues. To avoid this mistake, double-check that all required fields are filled out completely before submitting the form. Additionally, consider verifying the supervisor's credentials to ensure they are current and relevant.
Failing to indicate whether the supervisor's voicemail is confidential can create privacy concerns and hinder effective communication. It is important to clarify this aspect to ensure that sensitive information is handled appropriately. To prevent this oversight, take a moment to review the voicemail settings and clearly mark the confidentiality status on the form. This will help maintain the integrity of the communication process.
Neglecting to list additional services that the member is receiving can result in an incomplete understanding of the member's overall treatment plan. This information is crucial for ensuring coordinated care and avoiding potential conflicts in treatment. To avoid this mistake, make a comprehensive list of all services the member is currently receiving and include them in the request. Regularly updating this information can also help keep all providers informed.
Not confirming collaboration with other providers can lead to fragmented care and miscommunication among the treatment team. It is vital to ensure that all providers are aware of each other's involvement in the member's care. To mitigate this issue, actively reach out to other providers to discuss the treatment plan and document this collaboration on the form. This proactive approach fosters a more integrated treatment experience for the member.
Failing to meet the essential elements for Autism Spectrum Disorder can result in an incomplete or ineffective treatment request. It is crucial to adhere to the specific criteria outlined for ASD to ensure that the request is valid and actionable. To avoid this mistake, familiarize yourself with the essential elements required for ASD and ensure that all necessary documentation is included. Regular training and updates on these criteria can also enhance compliance.
Failing to include specific areas of impairment can lead to an incomplete understanding of the patient's needs. It is essential to provide comprehensive supporting data that illustrates the challenges faced by the individual. To avoid this mistake, ensure that all relevant information is gathered and clearly documented. Regularly review the patient's history and current functioning to identify and articulate these areas effectively.
Standardized assessment results are critical for justifying the need for treatment and demonstrating the patient's current level of functioning. Omitting these results can weaken the request and delay necessary services. To prevent this oversight, always include the most recent assessment data and ensure it is clearly referenced in the treatment request. Collaborate with assessment professionals to ensure accuracy and completeness.
An individualized treatment plan is essential for outlining the specific interventions and strategies tailored to the patient's unique needs. Missing these details can result in a lack of clarity regarding the treatment approach. To avoid this issue, take the time to develop a thorough treatment plan that includes specific goals, methods, and timelines. Engage with the patient and their family to ensure the plan reflects their preferences and needs.
Providing insufficient supporting data for the requested hours of treatment can lead to misunderstandings and potential denials. It is important to justify the number of hours requested with clear evidence of the patient's needs and treatment goals. To mitigate this risk, include detailed explanations and data that correlate the requested hours with the patient's specific impairments and treatment requirements. Regularly review and update this information as needed.
Defining measurable goals is crucial for tracking progress and ensuring accountability in treatment. Failing to establish these goals can hinder the effectiveness of the treatment plan and leave parents without clear expectations. To avoid this mistake, work collaboratively with parents to set specific, measurable, achievable, relevant, and time-bound (SMART) goals. Regularly review these goals with parents to ensure they remain aligned with the patient's progress and needs.
Omitting the criteria for titration and discharge can lead to delays in treatment approval and may result in the denial of the request. It is essential to provide clear and specific criteria that justify the need for titration and the conditions under which discharge will occur. To avoid this mistake, carefully review the treatment plan and ensure that all relevant criteria are documented. Consulting with clinical staff to confirm the criteria can also enhance the completeness of the request.
Not addressing barriers to providing information can hinder the review process and may lead to incomplete assessments. It is important to identify and document any challenges that may affect the ability to gather or submit necessary information. To prevent this issue, take the time to discuss potential barriers with the team and include them in the form. This transparency can facilitate a smoother review process and improve communication with the reviewing body.
Neglecting to read the important information section can result in missing critical instructions or requirements that are essential for the completion of the form. This oversight may lead to errors or omissions that could delay the processing of the request. To avoid this mistake, always take the time to thoroughly read all sections of the form, especially the important information section, before filling it out. Familiarizing yourself with the requirements can ensure that all necessary information is included.
Failing to provide a signature or title can render the form invalid and may result in processing delays. It is crucial to ensure that the individual completing the form signs it and includes their professional title to verify their authority. To avoid this mistake, double-check the form before submission to confirm that all required signatures and titles are present. Implementing a checklist for form completion can help ensure that no critical elements are overlooked.
Utilizing this form for a new precertification request instead of its intended purpose can lead to confusion and mismanagement of requests. This form is specifically designed for ABA treatment requests, and using it incorrectly may result in delays or denials. To prevent this mistake, ensure that you are using the correct form for the specific purpose intended. Always verify the form's purpose and guidelines before submission to ensure compliance with the requirements.
Submitting the form through an incorrect channel can lead to delays in processing and potential denial of services. It is crucial to follow the specified submission guidelines outlined in the instructions. To avoid this mistake, always verify the submission method, whether it is via email, fax, or an online portal, and ensure that you are using the most current version of the form. Double-check the contact information provided to ensure that your submission reaches the appropriate department.
Failing to submit the required documentation alongside the form can result in incomplete applications and subsequent delays. Ensure that all necessary supporting documents are included as specified in the instructions. To prevent this issue, create a checklist of required documents before submission and confirm that each item is attached. Additionally, consider keeping copies of all submitted materials for your records, which can be helpful in case of any follow-up inquiries.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out BHVH with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills outpatient-behavioral-health-bh-aba-assessment-precert forms, ensuring each field is accurate.