Fill out credentialing forms
with AI.
Credentialing forms are the backbone of healthcare administrative standards, ensuring that every practitioner operating within a facility or network meets specific educational and professional benchmarks. These documents collect comprehensive data, including medical education, residency training, board certifications, and professional liability history. By centralizing this information, healthcare organizations can maintain high standards of patient safety and comply with state regulations. Accurate documentation is essential not only for legal compliance but also for securing insurance reimbursement and maintaining the integrity of the medical community.
By continuing, you acknowledge Instafill's Privacy Policy and agree to get occasional product update and promotional emails.
About credentialing forms
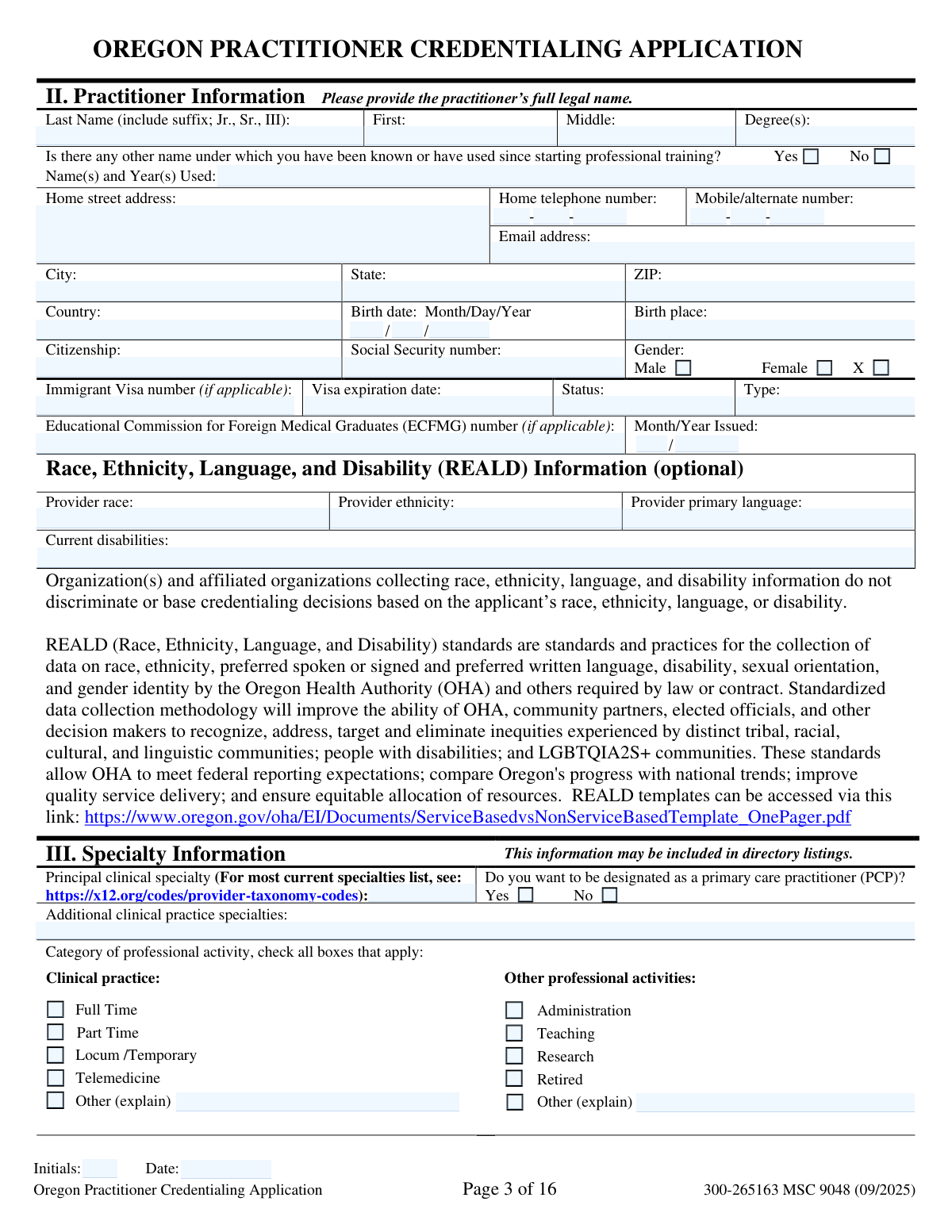
Healthcare providers, including physicians, dentists, and allied health professionals, typically encounter these forms when applying for hospital privileges or enrolling with insurance panels. For example, standardized applications like the Oregon Practitioner Credentialing Application are used across entire states to streamline the verification process for hospitals and health plans. Because even minor omissions or inaccuracies can delay a practitioner’s ability to work or lead to the denial of privileges, completing these forms with precision is critical for career continuity. Tools like Instafill.ai use AI to accurately and securely populate these forms in under 30 seconds, helping practitioners manage their administrative requirements with minimal manual effort.
Forms in This Category
- Enterprise-grade security & data encryption
- 99%+ accuracy powered by AI
- 1,000+ forms from all industries
- Complete forms in under 60 seconds
How to Choose the Right Form
Navigating medical credentialing can be complex, but for healthcare practitioners in Oregon, the process is largely standardized. Whether you are a physician, nurse practitioner, or another licensed provider, selecting the correct documentation is the first step toward securing hospital privileges or joining an insurance network.
The Universal Choice for Oregon Providers
If you are practicing within the state of Oregon, the primary document you will need is the Oregon Practitioner Credentialing Application (including Attachment A: Professional Liability Action Detail). This form was developed by the Advisory Committee on Physician Credentialing Information (ACPCI) to satisfy the requirements of House Bill 2144.
This single, comprehensive application is accepted by:
- Hospitals and surgery centers for facility privileges.
- Health plans and insurance networks for provider enrollment.
- State-mandated credentialing bodies across the state.
When to Use This Form
You should select the Oregon Practitioner Credentialing Application if you are:
- Applying for New Privileges: Use this for your initial application to a new healthcare facility or health plan within Oregon.
- Re-credentialing: Most organizations require an updated version of this form every two to three years to maintain your status.
- Updating Professional History: If you have had changes in your education, work history, or licensure, this form serves as the official record of your qualifications.
Key Components to Complete
Because this form is a legal attestation, accuracy is critical. Omissions or misstatements can lead to a denial of privileges. Ensure you have your NPI, DEA/CSR numbers, and a complete history of your medical education and facility affiliations ready.
If you have any history of professional liability claims, you must also complete Attachment A: Professional Liability Action Detail, which is included as part of the standard packet. Using this standardized form ensures that you meet the regulatory requirements of Oregon law while saving time by using a format recognized by all major healthcare entities in the state.
Form Comparison
| Form | Purpose | Who Files It | Key Requirements |
|---|---|---|---|
| Oregon Practitioner Credentialing Application (including Attachment A: Professional Liability Action Detail) | Standardized statewide application for credentialing with Oregon hospitals and health plans. | Healthcare practitioners applying for facility privileges or insurance network participation in Oregon. | Detailed history of education, licensure, work experience, peer references, and liability insurance. |
Tips for credentialing forms
Discrepancies between your CV, state licenses, and the application can significantly delay your approval. Double-check that dates of education and previous employment match exactly across all submitted documents to avoid flags during the verification process.
Credentialing committees often scrutinize gaps in employment or training that exceed 30 days. Providing a brief but clear explanation for any interruptions in your professional timeline prevents unnecessary follow-up inquiries and speeds up the review.
If you have a history of professional liability actions, use the required attachments to provide comprehensive details. Incomplete information regarding past claims is a frequent cause for application rejection or lengthy delays in granting privileges.
Answering 'No' to a question that should be 'Yes' can be interpreted as a material misstatement, even if it was an honest mistake. Take your time with the legal and ethical sections to ensure your responses are truthful and reflect your current standing.
Before starting, gather digital copies of your DEA registration, NPI number, and board certifications. Having these identifiers ready allows you to fill out extensive healthcare forms without searching through physical files for every new application.
AI-powered tools like Instafill.ai can complete these complex credentialing forms in under 30 seconds with high accuracy. Your sensitive professional data stays secure during the process, making it a highly efficient way to manage multiple medical applications.
Standardized forms like the Oregon Practitioner Application should not be altered or re-typed to ensure they meet state regulatory standards. Use a digital filling tool that maps data directly into the existing fields to keep the document’s integrity intact.
Frequently Asked Questions
Credentialing forms are used by hospitals, health plans, and medical groups to verify a practitioner’s qualifications, training, and professional history. This process ensures that healthcare providers meet specific standards of competency and safety before they are granted clinical privileges or allowed to participate in insurance networks.
This application is intended for healthcare practitioners seeking to practice in Oregon hospitals or join Oregon-based health insurance plans. It is used by physicians, nurse practitioners, physician assistants, and other licensed healthcare professionals to provide a comprehensive record of their professional background.
Oregon utilizes a standardized form, developed following House Bill 2144, to streamline the administrative process for both practitioners and healthcare organizations. By using a uniform document, the state reduces the burden of redundant paperwork, allowing providers to submit the same core information to multiple entities.
Practitioners generally need to have their educational transcripts, board certifications, state licenses, DEA registrations, and National Provider Identifier (NPI) numbers ready. Additionally, documentation regarding professional liability insurance coverage and a detailed work history are essential for completing the application accurately.
Yes, AI tools like Instafill.ai can be used to fill out complex credentialing forms in under 30 seconds. These tools accurately extract data from your CV, licenses, and other source documents to populate the form fields automatically, reducing the risk of manual entry errors.
Manually completing a comprehensive credentialing application can take several hours due to the level of detail required. However, using AI-powered automation allows you to complete the entire process in less than a minute by mapping your existing professional data directly into the standardized PDF.
It is recommended to start the credentialing process as early as possible, often three to six months before your anticipated start date. Because the verification of education, peer references, and hospital affiliations can take significant time, early submission helps prevent delays in beginning clinical work.
Attachment A, or the Professional Liability Action Detail, is used to provide specific information regarding any past or pending malpractice claims or professional liability actions. If you have a history of such actions, this supplement must be completed and submitted alongside the main application to ensure full disclosure.
Completed forms are typically submitted directly to the medical staff office of the hospital where you are seeking privileges or to the provider relations department of the health plan you wish to join. Since this is a standardized form, you may need to send copies to multiple organizations depending on your specific practice requirements.
Most credentialing forms require a continuous work history, often covering the last five to ten years. If there are gaps, you are generally required to provide a brief explanation for the period of inactivity to ensure there are no undisclosed issues or professional lapses.
Providing false, misleading, or incomplete information can lead to the denial of your application or the termination of your existing privileges and insurance contracts. Accuracy is critical, as healthcare organizations are legally and ethically required to verify the authenticity of all data provided during the credentialing process.
Glossary
- Credentialing
- The formal process of verifying a healthcare provider's qualifications, including education, training, and professional history, to ensure they meet standards for providing patient care.
- NPI (National Provider Identifier)
- A unique 10-digit identification number issued to healthcare providers in the United States by the Centers for Medicare and Medicaid Services (CMS).
- DEA Number
- A registration number assigned by the U.S. Drug Enforcement Administration that allows healthcare practitioners to prescribe controlled substances.
- Attestation
- A legally binding statement where the applicant signs to confirm that all information provided in the form is true, accurate, and complete.
- CME (Continuing Medical Education)
- Ongoing educational activities required for healthcare professionals to maintain their licenses and stay current with medical practices and technology.
- CSR (Controlled Substance Registration)
- A state-level registration required in some jurisdictions for practitioners to prescribe or dispense controlled substances, often used alongside federal DEA registration.
- Privileges
- The specific clinical tasks, procedures, or treatments a practitioner is authorized to perform within a specific hospital or healthcare facility.
- ACPCI (Advisory Committee on Physician Credentialing Information)
- The Oregon-based committee responsible for developing and maintaining the standardized credentialing application used by hospitals and health plans throughout the state.