Yes! You can use AI to fill out Ankle Conditions Disability Benefits Questionnaire
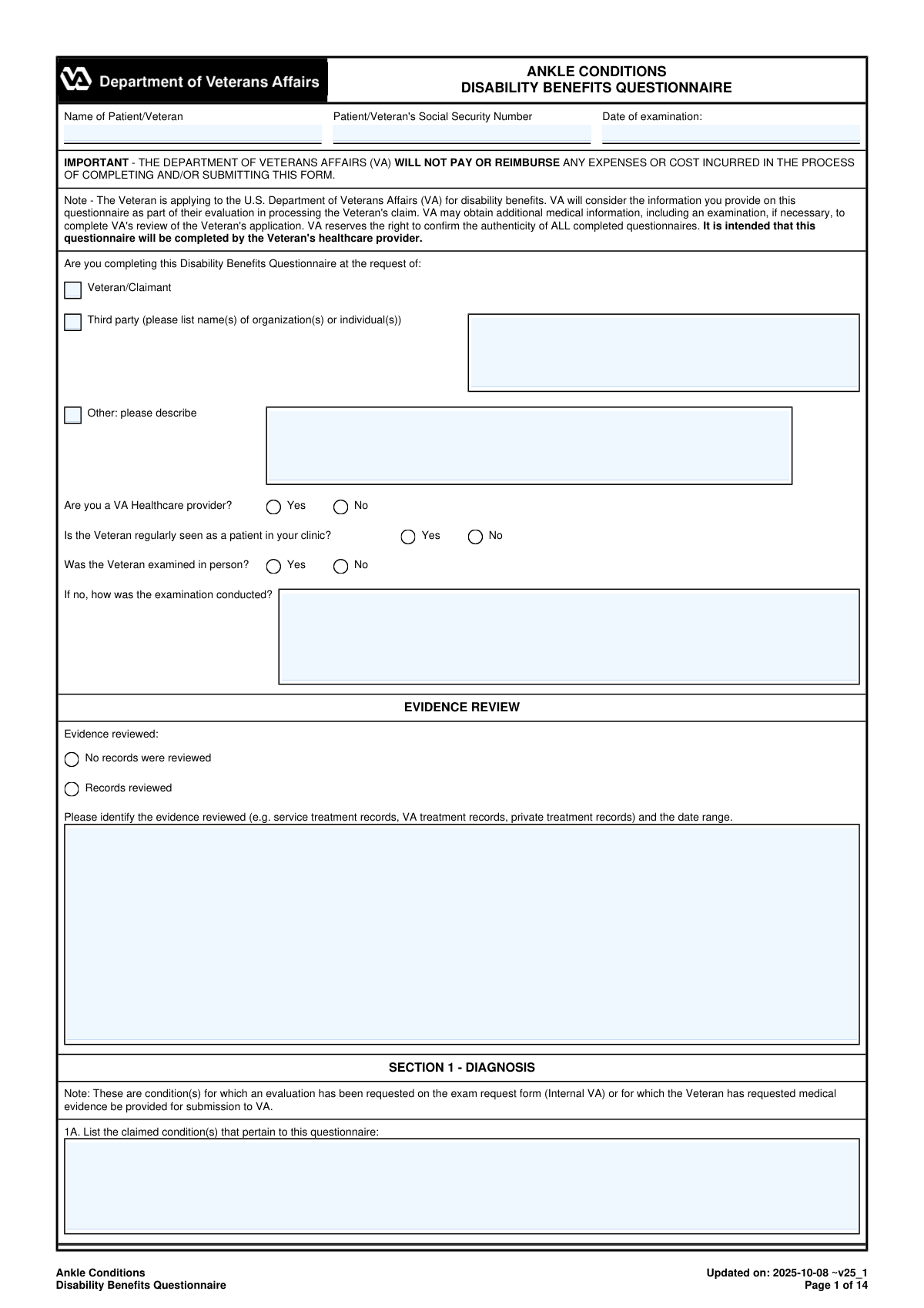
The Ankle Conditions DBQ is an official VA medical questionnaire intended to be completed by a qualified healthcare provider to support a Veteran’s VA disability benefits claim involving ankle conditions. It captures standardized clinical information such as diagnoses (with ICD codes), medical history, flare-ups, instability testing, range-of-motion measurements, imaging results, assistive device use, and occupational functional impact. Because VA disability ratings depend heavily on objective findings and functional loss, a complete and accurate DBQ can be critical evidence in establishing service connection and determining the correct rating level. The form also includes an examiner certification and signature section, and VA may verify the authenticity of submitted DBQs.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out VA DBQ (Ankle Conditions) using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Ankle Conditions Disability Benefits Questionnaire |
| Number of pages: | 14 |
| Filled form examples: | Form VA DBQ (Ankle Conditions) Examples |
| Language: | English |
| Categories: | healthcare forms, VA forms, disability forms, veteran forms, medical assessment forms, medical disability forms, medical forms, benefit forms |
Instafill Demo: filling out a legal form in seconds
How to Fill Out VA DBQ (Ankle Conditions) Online for Free in 2026
Are you looking to fill out a VA DBQ (ANKLE CONDITIONS) form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your VA DBQ (ANKLE CONDITIONS) form in just 37 seconds or less.
Follow these steps to fill out your VA DBQ (ANKLE CONDITIONS) form online using Instafill.ai:
- 1 Enter identifying information (Veteran/patient name, SSN, date of exam) and indicate who requested the DBQ and whether the examiner is a VA provider; document whether the exam was in-person or how it was conducted.
- 2 Complete the Evidence Review section by selecting whether records were reviewed and listing the types of records (service, VA, private) and the date ranges reviewed.
- 3 Fill out Section 1 (Diagnosis) by listing claimed ankle conditions, selecting all applicable diagnoses, specifying side affected (right/left/both), and adding ICD codes and diagnosis dates; add any additional ankle-related diagnoses as needed.
- 4 Document Section 2 (Medical History) including onset/course, flare-ups (frequency, duration, triggers, severity), functional loss with repeated use, and any history of ankle instability described by the Veteran.
- 5 Complete Section 3 (ROM and Functional Limitation) by recording active and passive ROM for each ankle, noting pain on weight-bearing/nonweight-bearing, performing repetitive-use testing, and providing estimated ROM loss for repeated use over time and flare-ups with supporting rationale.
- 6 Finish remaining clinical sections as applicable: muscle atrophy measurements, ankylosis details, joint stability tests (anterior drawer/talar tilt), additional conditions (shin splints, Achilles issues, malunion, talectomy), surgeries and residuals, scars/other findings, assistive devices, and diagnostic imaging results.
- 7 Describe functional impact on work-related activities (standing, walking, lifting, etc.), add any remarks, then complete the examiner certification with signature, credentials, specialty, contact information, NPI, license details, and date signed before generating the final submission-ready document.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable VA DBQ (Ankle Conditions) Form?
Speed
Complete your VA DBQ (Ankle Conditions) in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 VA DBQ (Ankle Conditions) form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form VA DBQ (Ankle Conditions)
This DBQ provides medical evidence about a Veteran’s ankle condition(s) for the VA to consider when evaluating a disability benefits claim. The VA may use it along with other records to decide service connection and the disability rating.
The form is intended to be completed by the Veteran’s healthcare provider (examiner). The Veteran can provide history and symptom descriptions, but the clinician must document exam findings, testing, and certify the report.
No. The form states that VA will not pay or reimburse any expenses or costs incurred to complete and/or submit the DBQ.
The form asks whether the Veteran was examined in person, and if not, it requires an explanation of how the examination was conducted. If an in-person exam is not performed, the examiner should clearly document the method and any limitations.
The examiner should indicate whether records were reviewed and list what was reviewed (e.g., service treatment records, VA treatment records, private records) and the date range. If no records were reviewed, that must be checked explicitly.
The DBQ includes many ankle-related diagnoses (e.g., ligament sprains, tendonitis, arthritis types, ankylosis, gout, bursitis, osteochondral injury, ankle replacement) and allows “Other” diagnoses. The examiner should also specify the side affected (right/left/both), ICD code, and date of diagnosis when available.
The examiner can select that the Veteran does not have a current diagnosis associated with the claimed condition(s) and must explain the findings and reasoning in the Remarks section. Symptom history can still be documented, but the DBQ requires clarity on whether a diagnosable condition is present.
If flare-ups are reported, the examiner should record the Veteran’s description, including frequency, duration, triggers, relief measures, severity, and functional impact. The ROM section also asks whether flare-ups significantly limit function and requests estimated ROM during flare-ups based on the Veteran’s statements and other evidence.
The form requests active and passive ROM for plantar flexion and dorsiflexion, and it asks the examiner to note pain on active vs. passive motion and on weight-bearing vs. nonweight-bearing. If ROM testing cannot be performed or is medically contraindicated, the examiner must explain why.
Repetitive-use testing involves at least three repetitions of ROM to see if function or ROM decreases after repeated movement. If the Veteran cannot perform it, the examiner must explain the reason, and the form still asks for opinions about functional loss after repeated use over time based on available evidence.
The DBQ still requires the examiner to estimate additional functional loss/ROM during flare-ups and after repeated use over time using “procurable information,” including the Veteran’s lay statements, medical records, and clinical expertise. If an estimate cannot be provided, the examiner must give a case-specific explanation (not a general statement).
Section 6 includes the Anterior Drawer Test and Talar Tilt Test and asks whether there is excessive/asymmetric motion or lack of a firm endpoint. If testing is “unable to test,” the examiner must explain why and indicate whether instability is still suspected.
They can be addressed in Section 7, which asks about shin splints (MTSS), stress fractures, Achilles conditions, malunion of calcaneus/talus, or talectomy. The form also notes that if shin splints are diagnosed with compartment syndrome, the Muscles questionnaire should be completed instead of this DBQ.
Section 8 asks the examiner to identify surgeries, provide dates, and describe residuals (including severity categories for total ankle replacement). For arthroscopic or other ankle surgery, the type of surgery, date, and residual symptoms/limitations should be documented.
Imaging is required to confirm degenerative (osteoarthritis) or post-traumatic arthritis, and the DBQ asks whether arthritis is documented and on which side. Once arthritis has been documented by imaging (even in the past), the form notes that additional imaging is not required by VA solely to show worsening.
Compliance VA DBQ (Ankle Conditions)
Validation Checks by Instafill.ai
1
Patient/Veteran Identifiers Present and Properly Formatted
Validate that the Patient/Veteran name and Social Security Number (SSN) fields are not blank. SSN should be exactly 9 digits (optionally formatted as XXX-XX-XXXX) and must not contain letters or invalid characters. This is critical for matching the questionnaire to the correct Veteran record; if it fails, the submission should be rejected or routed to manual review due to high risk of mis-association.
2
Examination Date and Signature Date Validity
Ensure 'Date of examination' and 'Date signed' are present, valid calendar dates, and not in the future. Also validate that the signature date is on or after the examination date (or require an explanation if not). If validation fails, the form should be flagged because VA adjudication depends on a credible timeline of evaluation and attestation.
3
Requestor Type Selection and Conditional Third-Party Details
Require exactly one requestor type to be selected: Veteran/Claimant, Third party, or Other. If 'Third party' is selected, at least one organization/individual name must be provided; if 'Other' is selected, a description must be provided. If missing or multiple selections occur, the submission should be blocked because provenance of the DBQ is unclear.
4
In-Person Exam vs. Remote Exam Explanation Consistency
If 'Was the Veteran examined in person?' is marked 'No', require the 'how was the examination conducted' field to be completed with a meaningful method (e.g., telehealth, records review only). If 'Yes' is selected, the remote-method field should be empty or ignored to prevent contradictory documentation. Failures should trigger a hard error or manual review because exam modality affects evidentiary weight.
5
Evidence Review Selection Requires Evidence Details
If 'Records reviewed' is selected, require the evidence description and date range to be populated (e.g., VA treatment records, STRs, private records, and approximate dates). If 'No records were reviewed' is selected, the evidence description/date range should be blank. If inconsistent, flag the submission because it undermines the basis for medical opinions and ROM estimates.
6
Claimed Conditions (Section 1A) Completeness
Validate that at least one claimed condition is listed in Section 1A (free text or structured entry), unless the system explicitly allows a blank claim list with a required remark explaining why. This ensures the DBQ is tied to a specific contention and prevents orphaned medical data. If missing, the form should be rejected as incomplete.
7
Diagnosis Selection vs. 'No Current Diagnosis' Mutual Exclusivity
Enforce that the checkbox 'The Veteran does not have a current diagnosis...' cannot be selected at the same time as any specific diagnosis in Section 1B. If 'no diagnosis' is selected, require a remarks entry explaining findings and reasons as instructed. If violated, the submission should be blocked because it creates a direct clinical contradiction.
8
Diagnosis Side Affected and ICD Code/Date Requirements
For each selected diagnosis, require a side affected (Right/Left/Both) and validate that ICD code (if captured) matches an acceptable ICD-10 format (e.g., letter + 2 digits + optional decimals). Require a diagnosis date that is a valid date or an allowed approximate format per system rules (e.g., YYYY-MM or YYYY). If missing/invalid, flag for correction because side and coding drive rating logic and downstream analytics.
9
Other Diagnosis Fields Require Specification and Side
If any 'Other (specify)' or 'Other diagnosis #1/#2/#3' is used, require the diagnosis text to be non-empty and a side affected to be selected. Prevent entries like 'N/A', 'unknown', or single-character placeholders unless accompanied by a clarifying remark. If validation fails, the form should be returned because unspecified diagnoses cannot be adjudicated or coded.
10
Flare-Ups and Functional Loss Conditional Narratives
If Section 2B (flare-ups) is 'Yes', require a narrative covering at least frequency and duration (and ideally precipitating/alleviating factors) rather than blank text. If Section 2C (functional loss) is 'Yes' or Section 2D (instability history) is 'Yes', require the Veteran’s description in their own words. If missing, flag as incomplete because these statements are required to support DeLuca/Sharp considerations and stability evaluation.
11
ROM Testing Status Requires Explanation When Not Performed
For each ankle, if ROM is marked 'Unable to test' or 'Not indicated', require an explanation describing why testing could not be performed or was contraindicated. If ROM is outside normal but stated to be normal for the Veteran for non-ankle reasons, require a description of the reason (e.g., neurologic disease) to justify the variance. If absent, the submission should be flagged because ROM is a core rating element.
12
ROM Degree Values Are Numeric and Within Physiologic Bounds
Validate that plantar flexion and dorsiflexion endpoints (active, passive, repetitive-use, repeated-use-over-time estimates, and flare-up estimates) are numeric values in degrees. Enforce reasonable bounds (e.g., plantar flexion 0–90, dorsiflexion -20–50) and disallow non-numeric text in degree fields. If out of range or non-numeric, block or route to manual review to prevent corrupted rating calculations.
13
Passive ROM 'Same as Active' vs. Entered Values Consistency
If 'Same as active ROM' is selected for passive ROM, the passive degree fields should be empty or automatically mirror the active values, not conflict with them. If 'Same as active' is not selected, passive ROM degree fields must be provided (or an explicit reason why not). Failures should be flagged because inconsistent passive/active ROM undermines exam reliability.
14
Pain/Functional Loss Logic and Required Comments
If 'Is there evidence of pain?' is 'Yes', require at least one applicable context (weight-bearing, nonweight-bearing, active, passive, rest) to be selected. If 'Causes functional loss' is checked, require a non-empty comment describing how pain contributes to functional loss; if 'Does not result in/cause functional loss' is checked, ensure 'Causes functional loss' is not also checked. If inconsistent, flag because pain findings directly affect functional assessment.
15
Repetitive-Use Testing and Post-Test ROM Conditional Requirements
If the Veteran is not able to perform repetitive-use testing (3B = No), require an explanation. If additional loss after three repetitions is 'Yes', require the post-test ROM endpoints and at least one factor causing functional loss (pain, fatigability, weakness, etc.). If missing, the form should be returned because repetitive-use findings are required for accurate functional limitation documentation.
16
Ankylosis Presence Requires Severity and Angle Consistency
If ankylosis of the ankle is 'Yes', require a severity category selection and require the ankylosis angle in degrees (plantar flexion and/or dorsiflexion as applicable). If ankylosis is 'No', enforce that the angle section is marked 'N/A' and no angles are entered. If inconsistent, flag because ankylosis drives distinct rating criteria and must be unambiguous.
Common Mistakes in Completing VA DBQ (Ankle Conditions)
People often leave the header fields blank or enter identifiers that don’t match the Veteran’s claim file (e.g., nickname, transposed SSN digits, or missing exam date). This can cause the DBQ to be rejected, misfiled, or delayed because VA cannot reliably associate it with the correct claimant and encounter. Always enter the Veteran’s full legal name, the correct SSN (or VA-required identifier), and the actual date the examination occurred, then double-check against the referral/records.
A common error is checking a box without listing the third-party organization name(s) or leaving the “Other” description blank. This creates ambiguity about the purpose and provenance of the report and may trigger follow-up requests to confirm authenticity. If “Third party” is selected, list the organization/individual exactly; if “Other,” provide a clear description (e.g., attorney request, employer, insurance).
Clinicians sometimes mark “Was the Veteran examined in person? No” but fail to describe how the exam was conducted (telehealth, records review only, phone interview). VA ROM and stability findings are heavily dependent on exam method, and missing details can reduce the probative value of the DBQ. If not in-person, document the modality, limitations, and what objective elements could not be performed.
Many submissions check “Records reviewed” but don’t list which records or the date range, or they check “No records were reviewed” while later citing imaging/notes. This inconsistency can undermine credibility and lead VA to discount the opinion or request clarification. List the specific sources (service treatment records, VA treatment records, private ortho notes, imaging reports) and the exact date range reviewed.
A frequent mistake is checking a diagnosis but not completing the required details: side affected, ICD code, and date of diagnosis, or selecting “Both” while only describing unilateral symptoms. VA ratings depend on accurate laterality and a clear diagnostic timeline, and incomplete diagnosis fields often prompt rework. For each diagnosis, specify right/left/both, provide the ICD code if requested, and use an approximate diagnosis date if exact is unknown (not “N/A” unless truly not applicable).
Some providers check “The Veteran does not have a current diagnosis…” and then leave the Remarks section empty. VA needs a medical explanation (e.g., resolved condition, symptoms without diagnosable pathology, conflicting prior diagnoses) to understand why no diagnosis applies. If you select no diagnosis, explain the clinical findings, relevant negative tests, and why prior labels do or do not apply.
People often write “has flare-ups” or “pain with walking” without documenting frequency, duration, triggers, alleviating factors, severity, and functional impact in the Veteran’s own words. This leads to inadequate information for estimating functional loss during flare-ups and after repeated use over time, which is central to musculoskeletal ratings. Capture specifics (e.g., “2–3 times/week, lasts 1–2 days, triggered by stairs, relieved by rest/brace, cannot stand >10 minutes”).
Common data-entry issues include leaving ROM endpoints blank, entering ranges as text (e.g., “limited”), using percentages, or recording values that exceed normal without explanation. Another frequent inconsistency is marking “All normal” while documenting painful motion and reduced endpoints, or failing to explain “Unable to test/Not indicated.” Always record plantar flexion and dorsiflexion endpoints in degrees for each ankle, reconcile checkboxes with the numeric values, and provide a clear reason if testing cannot be performed.
This DBQ specifically asks examiners to address pain on active and passive motion and on weight-bearing and nonweight-bearing, yet many forms only document one condition (e.g., active ROM only). Missing these elements can make the exam inadequate under VA expectations and may result in a new exam request. Ensure you indicate whether pain is present in each context, select the applicable checkboxes, and add comments describing whether pain causes functional loss.
A very common mistake is leaving the “estimate ROM in degrees” fields blank or writing “cannot determine without resorting to speculation” without a case-specific explanation and discussion of procurable evidence. VA expects an estimate based on the Veteran’s statements, records, and clinical judgment when feasible, and generic refusals often trigger remand/clarification. Provide best medical estimates in degrees and cite the Veteran’s reported limitations and any supporting records; if truly not feasible, explain specifically what information is missing and why it prevents an estimate in this case.
Providers sometimes select “Unable to test” for Anterior Drawer or Talar Tilt but do not explain why, and they also skip the follow-up question about whether instability is suspected. This leaves VA without a usable stability assessment and can affect ratings related to instability. If unable to test, document the reason (pain, guarding, recent surgery, risk of injury) and then state whether instability is suspected and why (history of giving way, brace use, prior sprains).
Submissions often check that surgery or assistive devices exist but omit dates, types, residuals, frequency of use, side, or the condition prompting the device; similarly, signatures, credentials, NPI/license, and contact info are frequently missing. These omissions can delay processing because VA may need to verify the examiner’s qualifications and understand residual functional impact. Include surgery type and date, describe residuals, specify device frequency and laterality, and complete all certification/signature and licensing identifiers exactly as requested.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out VA DBQ (Ankle Conditions) with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills ankle-conditions-disability-benefits-questionnaire forms, ensuring each field is accurate.