Yes! You can use AI to fill out Center for Infertility & Reproductive Surgery – New Patient Questionnaire and Patient/Guarantor Statement (Brigham and Women’s Hospital, Department of Obstetrics and Gynecology)
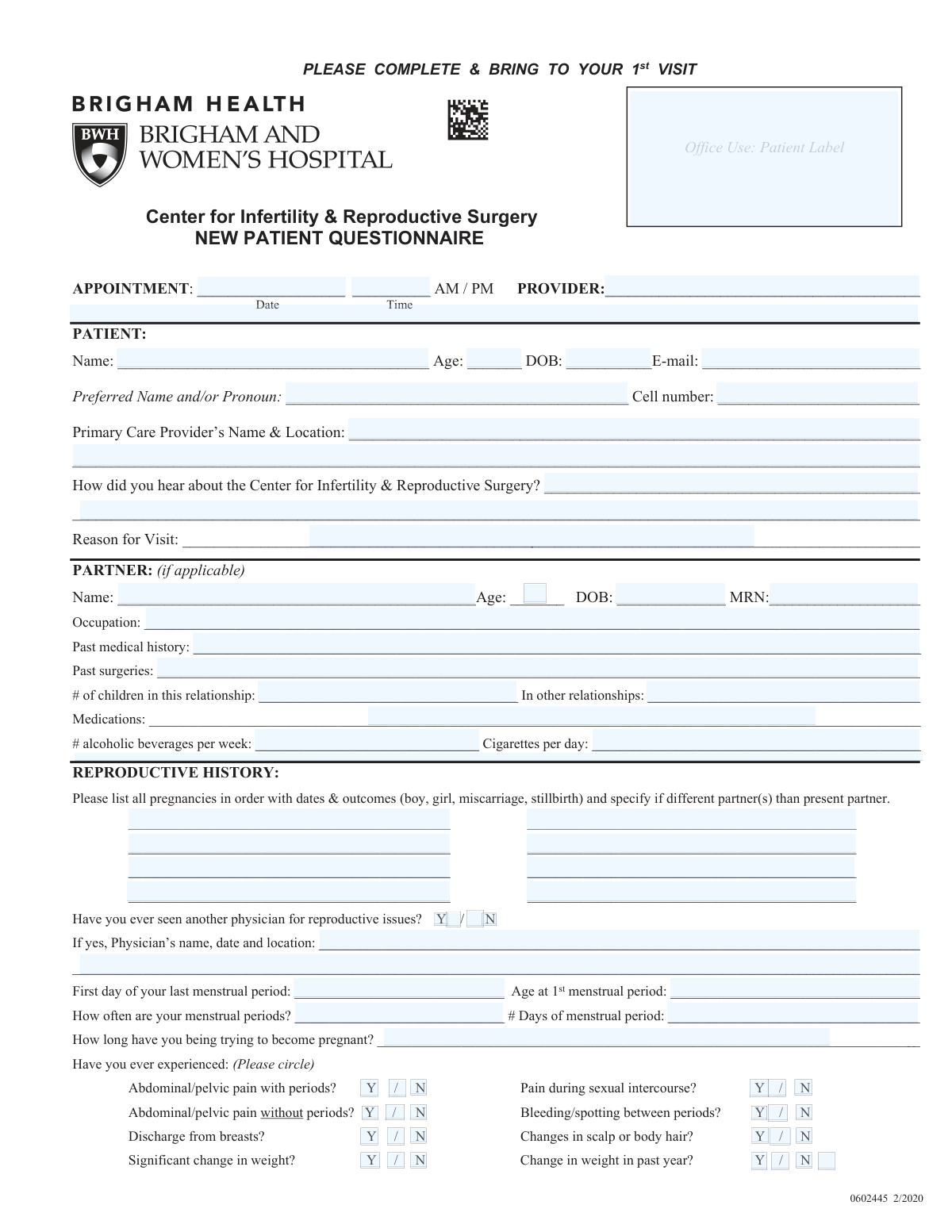
This form packet is a fertility clinic new-patient intake questionnaire used to gather detailed information about the patient and (if applicable) their partner, including reproductive history, menstrual history, prior fertility testing/treatments, medical/surgical history, medications, allergies, family history, and social/health habits. It also includes a Patient/Guarantor Statement confirming the patient’s responsibility to understand insurance coverage, obtain authorizations/referrals, and pay applicable copays, deductibles, and non-covered charges. The information becomes part of the medical record and helps the care team plan appropriate infertility evaluation and treatment while documenting financial consent for services.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out CIRS New Patient Questionnaire using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Center for Infertility & Reproductive Surgery – New Patient Questionnaire and Patient/Guarantor Statement (Brigham and Women’s Hospital, Department of Obstetrics and Gynecology) |
| Number of pages: | 4 |
| Language: | English |
| Categories: | insurance forms, prior authorization forms, medical authorization forms, medical forms, OBGYN forms, patient intake forms, hospital forms, patient forms, PA state forms |
Instafill Demo: filling out a legal form in seconds
How to Fill Out CIRS New Patient Questionnaire Online for Free in 2026
Are you looking to fill out a CIRS NEW PATIENT QUESTIONNAIRE form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your CIRS NEW PATIENT QUESTIONNAIRE form in just 37 seconds or less.
Follow these steps to fill out your CIRS NEW PATIENT QUESTIONNAIRE form online using Instafill.ai:
- 1 Enter appointment details (date, time, provider) and complete patient identifiers and contact information (name, DOB, age, email, phone, PCP).
- 2 Fill in partner information (if applicable), including demographics, medical/surgical history, medications, children, and lifestyle factors (alcohol, smoking).
- 3 Complete reproductive and menstrual history: list all pregnancies with dates/outcomes, last menstrual period, cycle frequency/length, symptoms (pain, bleeding, discharge), and how long you’ve been trying to conceive.
- 4 Document prior infertility evaluation and diagnostic testing (e.g., blood tests, HSG, laparoscopy/hysteroscopy findings, semen analysis) and check any previous fertility treatments (IUI, IVF, ICSI, medications, etc.).
- 5 Provide gynecologic and general medical history: pap/mammogram history, STDs/PID/DES exposure, medical conditions checklist, past surgeries with dates, allergies, and current medications with dosages.
- 6 Complete family medical history and social/personal safety sections (marital status, stressors, smoking/alcohol/drug use, safety at home, falls/balance).
- 7 Review for accuracy, acknowledge the information becomes part of your medical record, then sign/date/time the consent statements and the Patient/Guarantor Statement (including written name and MRN if available).
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable CIRS New Patient Questionnaire Form?
Speed
Complete your CIRS New Patient Questionnaire in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 CIRS New Patient Questionnaire form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form CIRS New Patient Questionnaire
This questionnaire collects your medical, reproductive, and social history so your provider can evaluate fertility concerns and plan appropriate testing or treatment. It becomes part of your medical record and helps make your first visit more efficient.
The patient should complete the main sections, and the partner section should be completed if you have a partner involved in trying to conceive. If you do not have a partner or they are not participating, you can leave the partner section blank.
Complete it before your first visit and bring it with you to the appointment. The top section includes appointment date/time and provider, which you can fill in if known.
Have your menstrual history (last period date, cycle frequency), a list of current medications with doses, prior fertility testing/treatment details, and dates/results of Pap smear and mammogram if applicable. If you’ve had gynecologic surgery, bring a copy of the operative note as requested.
List all pregnancies in order with dates and outcomes (e.g., live birth boy/girl, miscarriage, stillbirth). If any pregnancy involved a different partner than your current partner, note that as well.
It means the first day you started bleeding in your most recent period (cycle day 1). If you’re unsure, provide your best estimate.
Write “irregular” or “no periods” and include any details you know (typical range of days between periods, when your last bleeding occurred, or any known diagnosis). This information helps your provider decide what testing may be needed.
Fill in any results you have (FSH, TSH, estradiol, prolactin, progesterone, immunity tests, semen analysis, HSG, biopsy, etc.). If you don’t know the numbers, you can write “unknown” and bring copies of prior records if available.
Check every treatment you have tried in the past (for example, Clomid/Serophene, IUI, IVF, ICSI, Lupron, birth control pills, etc.). If you’re unsure which medications you used, list what you remember in the space provided or attach a medication list from your prior clinic.
These factors can affect timing, sperm function, comfort with intercourse, and overall fertility planning. Answer as accurately as you can; if something is sensitive, you can discuss details privately with your provider.
List all surgeries and approximate dates, especially gynecologic procedures (e.g., laparoscopy, fibroid surgery, C-section). An operative note is the surgeon’s report describing what was done during surgery; the form asks you to bring a copy for gynecologic surgeries if possible.
For medications, include the name, dose, and how many times per day you take each (including vitamins and supplements if relevant). For allergies, list the allergen (medication/latex/etc.) and the reaction you have (e.g., rash, swelling, trouble breathing).
They help the clinic identify safety risks (such as feeling unsafe at home, fall risk, or relationship threats) and provide appropriate support. You should answer honestly; if you have concerns, you can ask to discuss them confidentially with your care team.
By signing, you give written permission for the clinic to access notes from mental health providers you may have seen, to support your reproductive care. You can revoke consent later, but the form notes that doing so may affect the clinic’s ability to provide certain reproductive services.
It confirms you are responsible for understanding your insurance coverage (including referrals/authorizations) and for paying required copays, deductibles, and non-covered services. It also states payment may be required in advance, any deposit is only an estimate, and the estimate can change based on services provided; the waiver is valid for one year from the signature date.
Compliance CIRS New Patient Questionnaire
Validation Checks by Instafill.ai
1
Appointment Date/Time and AM/PM Format Validation
Validates that the appointment date is a real calendar date (e.g., MM/DD/YYYY) and the time is in a valid format (e.g., HH:MM) with exactly one AM/PM selection. This is important for scheduling accuracy and to prevent missed or mis-timed visits. If invalid or missing, the submission should be flagged and the patient prompted to correct the date/time before the appointment can be confirmed.
2
Provider Name Required and Non-Placeholder Check
Ensures the PROVIDER field is completed with a real provider name and not left blank or filled with placeholders (e.g., underscores, 'N/A', or 'unknown'). Provider identification is required for routing the questionnaire to the correct clinical team and for medical record integrity. If validation fails, the form should be rejected for completion or routed to staff for reconciliation.
3
Patient Identity Completeness (Name, DOB, Age) and Consistency
Checks that the patient’s full legal name, date of birth, and age are provided and that age is consistent with DOB (within an acceptable tolerance based on current date). This prevents patient misidentification and reduces charting errors. If inconsistent or incomplete, the system should require correction and/or trigger an identity verification workflow.
4
Partner Section Conditional Completeness
If any partner fields are started (e.g., partner name, DOB, MRN, occupation), validates that the partner name and DOB (or age) are also provided and internally consistent. This is important because partner history and semen analysis/treatment history may be clinically relevant and must be attributable to the correct person. If partial data is entered without required identifiers, the system should prompt the user to either complete the partner section or clear it.
5
MRN Format Validation (Patient and Partner)
Validates that MRN values (patient and partner) match the organization’s expected format (e.g., numeric-only and correct length) and are not obviously invalid (all zeros, too short, or containing letters if not allowed). Correct MRNs are critical for matching the questionnaire to the correct medical record. If invalid, the system should block submission or mark the record as unmatched for manual review.
6
Email Address Format Validation
Ensures the patient email follows standard email syntax ([email protected]) and does not contain spaces or invalid characters. Email is often used for portal access, instructions, and follow-up communication. If invalid, the system should request correction or allow submission only if an alternate contact method (e.g., phone) is present.
7
Cell Phone Number Format and Length Validation
Validates that the cell number contains a valid phone pattern (e.g., 10 digits for US numbers, allowing punctuation like parentheses/dashes) and is not an obviously fake value (e.g., 000-000-0000). Reliable phone contact is essential for time-sensitive clinical communication and appointment coordination. If validation fails, the form should prompt for a corrected number or require an alternate contact method.
8
Yes/No Questions Must Have Exactly One Selection
For each Y/N item (e.g., smoking, drug use, safety questions, prior reproductive physician, STD history), validates that exactly one option is selected and that both are not selected or left ambiguous. These fields drive clinical risk screening and downstream workflows (e.g., counseling, referrals). If missing or conflicting, the system should require the user to choose a single answer before submission.
9
Conditional Detail Requirement for 'Yes' Responses
When a question is answered 'Yes' and a follow-up is requested (e.g., 'If yes, which drugs', 'If yes, what lubricants', 'If yes, physician’s name/date/location', abnormal pap smear treatment details), validates that the corresponding explanation field is completed. This ensures clinicians have actionable context rather than a bare affirmative response. If missing, the system should prompt for the required details or flag the submission as incomplete.
10
Menstrual History Date and Range Validation (LMP and Menarche Age)
Validates that the 'First day of your last menstrual period' is a real date and not in the future, and that 'Age at 1st menstrual period' is a plausible integer range (e.g., 8–20). Menstrual timing is central to fertility evaluation and treatment planning. If values are out of range or invalid, the system should request correction and flag for clinical review if the patient insists the value is correct.
11
Cycle Length and Period Duration Numeric Validation
Ensures 'How often are your menstrual periods?' is captured as a numeric cycle length in days (or a structured frequency) and '# Days of menstrual period' is a positive integer within a plausible range (e.g., 1–14). Standardized numeric values support clinical interpretation and analytics. If non-numeric or implausible, the system should prompt for clarification or convert to a structured format.
12
Trying-to-Conceive Duration Completeness and Plausibility
Validates that 'How long have you been trying to become pregnant?' is provided in a structured duration (months/years) and is not negative or implausibly large relative to patient age (e.g., longer than reproductive lifespan without explanation). This field is often used to determine infertility criteria and urgency of evaluation. If missing or unparseable, the system should require a corrected duration entry.
13
Alcohol and Tobacco Use Numeric and Cross-Field Consistency
Checks that '# alcoholic beverages per week' and 'Cigarettes per day' are numeric, non-negative, and within reasonable bounds, and cross-validates smoking answers (e.g., if 'Do you smoke? = No' then cigarettes/day should be blank or 0). Substance use impacts fertility and pregnancy risk counseling, so consistency matters. If inconsistent, the system should prompt the user to reconcile the Y/N response with the numeric quantity.
14
Reproductive History Entries Require Date and Outcome Structure
If pregnancies are listed, validates that each entry includes at minimum a date (or year) and an outcome (e.g., live birth, miscarriage, stillbirth) and optionally sex when provided, and that entries are in chronological order as requested. Structured pregnancy history is essential for accurate obstetric risk assessment and fertility planning. If entries are missing key components or are not parseable, the system should request re-entry in a standardized format.
15
Diagnostic Test Result Format Validation (Numeric Labs vs. Text Procedures)
Validates that lab values (FSH, TSH, Estradiol, Prolactin, Progesterone) are numeric (allowing decimals) and optionally include units, while procedure fields (HSG, biopsy, laparoscopic/hysteroscopic findings, semen analysis) accept text but should not be only placeholders. Correct formatting prevents misinterpretation and supports clinical decision-making. If a numeric field contains non-numeric text or an impossible value (e.g., negative), the system should flag it for correction or clinician review.
16
Signature, Printed Name, and Date/Time Completion for Consents and Financial Statement
Ensures required signatures are present for the clinical review acknowledgment and the Patient/Guarantor Statement, along with written/printed name and signature date (and time with AM/PM where requested). These elements are necessary for legal consent, authorization to access records, and financial responsibility acknowledgment. If any required signature or date is missing, the system should prevent final submission and mark the packet as incomplete.
Common Mistakes in Completing CIRS New Patient Questionnaire
People often skip the APPOINTMENT date/time, forget to circle AM vs PM, or write a time that doesn’t match what was scheduled. This can cause check-in delays, misrouting to the wrong provider, or staff needing to re-confirm details on arrival. Copy the appointment information directly from your confirmation message/portal and clearly mark AM or PM.
Because the form has separate areas for PATIENT and PARTNER, many people accidentally enter their own information in the partner section (or vice versa), or leave the partner section blank even when a partner is involved in fertility care. This can lead to incomplete clinical assessment and missing required testing history (e.g., semen analysis). Double-check whose name is at the top of the section and complete both sets of demographics and histories when a partner is part of the evaluation.
Patients frequently omit DOB/MRN, transpose digits, or write a preferred name where the legal name is needed for matching records. This can delay record retrieval, lab/result matching, and insurance processing. Enter your legal name as it appears on insurance/ID, add preferred name/pronouns in the designated field, and copy DOB/MRN carefully from prior visit paperwork or the patient portal.
The reproductive history asks for all pregnancies in order with dates and outcomes and to specify if a different partner was involved, but many people only list live births or omit miscarriages/terminations/chemical pregnancies. Incomplete pregnancy history can change the clinical interpretation of infertility causes and the recommended workup. Include every pregnancy event you know of, approximate dates if exact dates are unknown, the outcome, and note if the partner at that time was different.
Common errors include writing the expected next period instead of the first day of the last menstrual period (LMP), giving a range without clarity, or confusing cycle length with number of bleeding days. These details affect timing of labs/ultrasounds and interpretation of ovulatory function. Record the first day of your most recent period, provide average days between periods (cycle length), number of days you bleed, and estimate if you’re unsure (e.g., “about 28–30 days”).
The form relies heavily on Y/N choices (pain, symptoms, smoking, safety questions, prior reproductive physician), and people often check neither, circle both, or mark in the margin. This creates ambiguity and may require staff to re-ask sensitive questions during the visit. For every Y/N item, circle exactly one option and add brief details only when the form asks for them (e.g., physician name/date/location if “Yes”).
Many patients list only medication names (or only supplements) without dose and how many times per day, and list allergies without describing the reaction (e.g., rash vs anaphylaxis). This can lead to unsafe prescribing, missed drug interactions, or delays while staff clarifies. List every current medication and supplement with dose and frequency, and for each allergy include the specific reaction and approximate severity.
People often leave blanks, provide vague answers (“socially”), or use inconsistent units (e.g., drinks per month vs per week) even though the form asks for cigarettes per day and alcoholic beverages per week. Inaccurate reporting can affect fertility counseling, anesthesia/procedure planning, and medication choices. Convert to the requested units (average per week/per day) and, if you quit, note quit date and prior amount.
Patients frequently check treatments (IUI/IVF/ICSI, Clomid, gonadotropins) or list tests (HSG, semen analysis, laparoscopy) but don’t include dates, outcomes, or key findings. This can cause duplicate testing, missed abnormal results, and slower treatment planning. Add approximate dates and results where possible (e.g., “HSG 2023—tubes open”), and bring copies of operative notes and key reports as requested.
The family history section asks for ages and medical problems for multiple relatives, but many people leave it blank or provide only diagnoses without indicating which relative or age at diagnosis. Missing details can limit genetic risk assessment and screening recommendations. If you don’t know specifics, write “unknown” for that relative and include any partial information you do know (e.g., “father—diabetes, diagnosed in 40s”).
It’s common to sign one line but miss the date/time, forget the second patient signature attestation, or omit the guarantor statement signature/printed name/MRN. Missing signatures can prevent the clinic from accessing needed records (including mental health notes if applicable) and can delay registration or treatment scheduling. Before submitting, verify every signature block has a signature, printed name when requested, date, and time with AM/PM.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out CIRS New Patient Questionnaire with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills center-for-infertility-reproductive-surgery-new-pa forms, ensuring each field is accurate.