Yes! You can use AI to fill out Manulife Group Benefits Drug Prior Authorization Form (Wegovy/Semaglutide) – GL5197E - MLI (08/2025-WEGOV)
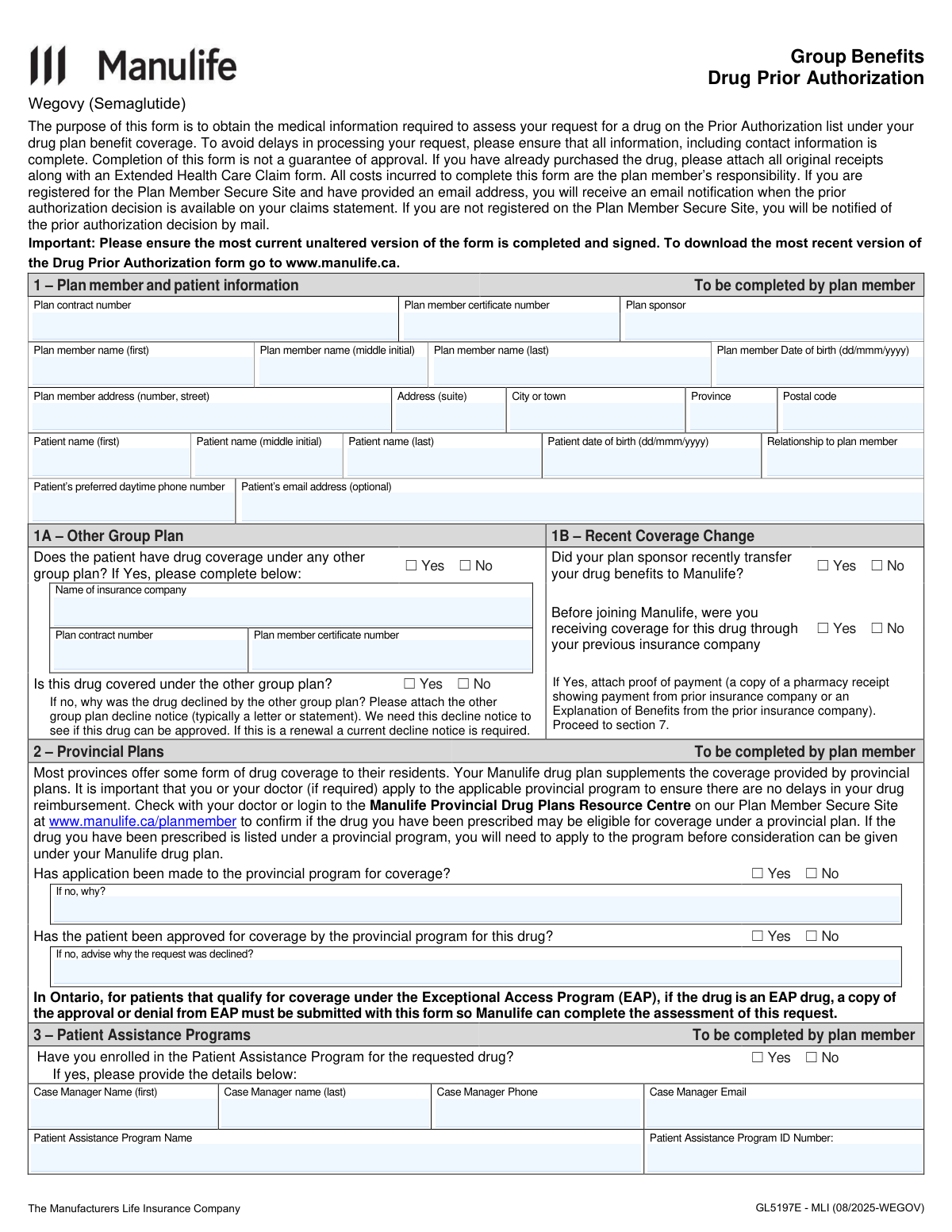
The Manulife Group Benefits Drug Prior Authorization form (GL5197E) is an insurer-required document used to request coverage approval for a medication on the plan’s prior authorization list—here, Wegovy (semaglutide). It collects plan member/patient identifiers, other insurance and provincial coverage details, patient assistance program information, and detailed clinical criteria and drug history completed by the prescribing physician. The form is important because incomplete or missing information can delay review, and submission does not guarantee approval; supporting documents (e.g., provincial program decisions, other plan decline notices, receipts) may be required. Today, this form can be filled out quickly and accurately using AI-powered services like Instafill.ai, which can also convert non-fillable PDF versions into interactive fillable forms.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out GL5197E (Wegovy) using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Manulife Group Benefits Drug Prior Authorization Form (Wegovy/Semaglutide) – GL5197E - MLI (08/2025-WEGOV) |
| Number of pages: | 6 |
| Language: | English |
| Categories: | insurance forms, prior authorization forms, Manulife forms, health benefit forms, authorization forms |
Instafill Demo: filling out a legal form in seconds
How to Fill Out GL5197E (Wegovy) Online for Free in 2026
Are you looking to fill out a GL5197E (WEGOVY) form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your GL5197E (WEGOVY) form in just 37 seconds or less.
Follow these steps to fill out your GL5197E (WEGOVY) form online using Instafill.ai:
- 1 Go to Instafill.ai and upload the Manulife Drug Prior Authorization form (GL5197E - Wegovy) or select it from the form library.
- 2 Enter plan member and patient details (contract/certificate numbers, sponsor, names, dates of birth, address, relationship, phone, and optional email).
- 3 Complete coverage coordination sections: indicate other group drug coverage and any recent transfer to Manulife, and add prior insurer details and required attachments (decline notice or proof of payment) if applicable.
- 4 Fill in provincial plan and patient assistance program information, including application/approval status and case manager/program identifiers when relevant.
- 5 Have the prescribing physician complete the medical information: drug strength/dosage, administration location, diagnosis selection (initial/renewal criteria), and required clinical measurements and eligibility questions.
- 6 Add drug history and physician information (license/college number, specialty, contact details), then apply the physician signature and date using Instafill.ai’s e-sign or signature tools as permitted.
- 7 Review for completeness, attach supporting documents, then submit via the Plan Member Secure Site “Submit a Claim” feature or print/export to mail/fax to Manulife’s Prior Authorization Team as instructed, keeping a copy for your records.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable GL5197E (Wegovy) Form?
Speed
Complete your GL5197E (Wegovy) in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 GL5197E (Wegovy) form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form GL5197E (Wegovy)
This form is used to collect the medical and coverage information Manulife needs to assess a request for a drug that is on your plan’s Prior Authorization list (e.g., Wegovy/semaglutide). Submitting the form helps Manulife decide whether the drug will be covered under your Group Benefits drug plan.
You (the plan member) complete Sections 1–3 and sign Section 7. The prescribing physician must complete Sections 4–6, including diagnosis details, drug history, and the physician signature.
No. The form states that completion is not a guarantee of approval—Manulife will review the information and make a coverage decision based on your plan rules and the medical criteria.
You’ll need your plan contract number, certificate number, plan sponsor (employer/organization), your personal details and address, and the patient’s details (if different from the plan member), including relationship and contact information.
Check “Yes” and provide the other insurer’s name, contract number, and certificate number, and indicate whether the drug is covered there. If the other plan declined the drug, attach the decline notice (and for renewals, a current decline notice is required).
Answer whether your plan sponsor transferred benefits to Manulife and whether you previously had coverage for this drug with the prior insurer. If you had coverage, attach proof of payment such as a pharmacy receipt showing payment by the prior insurer or an Explanation of Benefits.
Often, yes—Manulife notes that provincial plans may provide coverage first and your Manulife plan may supplement it. If the drug is eligible under a provincial program, you generally need to apply before Manulife can assess your request.
If the patient qualifies for Ontario EAP and the drug is an EAP drug, you must submit a copy of the EAP approval or denial with this form. Manulife uses that document to complete the assessment.
This section asks whether you enrolled in the manufacturer’s Patient Assistance Program and, if so, the case manager and program details. Enrollment isn’t stated as mandatory on the form, but providing details can help coordinate benefits and avoid delays.
The physician must select the diagnosis category (e.g., chronic weight management pediatric/adult initial or renewal, or non-fatal myocardial infarction risk reduction) and answer the related criteria questions such as baseline BMI/weight, response/benefit, comorbidities, and confirmation the dose will not exceed 2.4 mg once weekly and is not combined with other GLP-1 analogs.
The physician can select “Any Other Diagnosis” and must provide the specific diagnosis plus any Canadian clinical research supporting the use of the drug in your situation. This additional detail is required for Manulife to assess an off-pathway request.
The physician should list previous and current therapies for the diagnosis, including drug names, start/end dates, outcomes (intolerance/adverse event or inadequate response), and whether each medication will be continued with the new therapy. If no previous therapies were tried, the physician must check a reason (e.g., contraindication) and provide medical rationale.
If you’re registered on the Plan Member Secure Site and have an email address on file, you’ll receive an email notification when the decision is available on your claims statement. If you’re not registered, Manulife will notify you by mail.
You can submit using the “Submit a Claim” feature on the Plan Member Secure Site, or mail/fax it to Manulife’s Prior Authorization Team. Quebec residents mail to PO BOX 2580, Station B, Montreal QC H3B 5C6; outside Quebec mail to PO BOX 1653, Waterloo ON N2J 4W1; fax is 1-855-752-0404 for both.
Yes—AI tools like Instafill.ai can help auto-fill form fields accurately using the information you provide, saving time and reducing missed fields. If your PDF is flat/non-fillable, Instafill.ai can convert it into an interactive fillable form and then guide you to complete and export it for submission.
Compliance GL5197E (Wegovy)
Validation Checks by Instafill.ai
1
Required Plan Member Coverage Identifiers Present (Contract/Certificate/Sponsor)
Validates that Plan Contract Number, Plan Member Certificate Number, and Plan Sponsor are all provided and not left blank. These identifiers are required to locate the correct benefits plan and route the request to the right sponsor/coverage. If any are missing, the submission should be rejected or pended with a request for the missing identifiers because adjudication cannot proceed reliably.
2
Plan Member and Patient Name Completeness and Character Validation
Checks that first and last names for both plan member and patient are present, and that name fields contain only expected characters (letters, spaces, hyphens, apostrophes) and do not contain numbers or symbols. This reduces mismatches in member/patient identification and prevents downstream system errors. If validation fails, the form should be returned for correction and the record should not be created/updated.
3
Date of Birth Format and Validity (dd/mmm/yyyy) for Plan Member and Patient
Ensures Plan Member Date of Birth and Patient Date of Birth follow the required format (dd/mmm/yyyy, e.g., 05/JAN/2010) and represent real calendar dates. Correct DOB formatting is critical for eligibility checks, dependent validation, and clinical criteria (pediatric vs adult). If invalid or missing, the submission should be flagged as incomplete and held until corrected.
4
Age Consistency with Selected Diagnosis Path (Pediatric vs Adult)
Validates that the patient’s age derived from Patient Date of Birth is logically consistent with the diagnosis section selected (pediatric vs adult criteria). This prevents applying the wrong clinical rules and avoids inappropriate approvals/denials. If inconsistent (e.g., adult age with pediatric criteria), the submission should be pended for clarification or corrected diagnosis selection.
5
Canadian Address Validation for Plan Member (Province and Postal Code)
Checks that Province is selected/entered as a valid Canadian province/territory and that Postal Code matches Canadian format (A1A 1A1) and is consistent with the province when possible. Accurate address data is required for mail notifications and jurisdictional handling (e.g., Quebec routing). If invalid, the form should be rejected or pended because notifications and processing may fail.
6
Patient Preferred Daytime Phone Number Format Validation
Validates that the preferred daytime phone number is present and matches an acceptable phone format (e.g., 10-digit NANP with optional country code, parentheses, spaces, or hyphens). Contact information is required to resolve clinical/administrative questions quickly and avoid delays. If invalid or missing, the submission should be pended and the requester asked to provide a reachable number.
7
Email Address Format Validation (Optional Field)
If an email address is provided, verifies it conforms to standard email syntax (local@domain) and does not contain spaces or invalid characters. This supports secure site notifications and reduces failed communications. If invalid, the system should either reject the email value (while allowing submission) or pend if email is required for a chosen communication workflow.
8
Mutually Exclusive Yes/No Checkbox Enforcement (All Binary Questions)
Ensures that for each Yes/No question (e.g., other group plan coverage, transferred benefits, provincial application/approval, PAP enrollment, GLP-1 combination, dose exceeds 2.4 mg), exactly one option is selected. Selecting both or neither creates ambiguity and can lead to incorrect adjudication logic. If the rule is violated, the submission should be flagged as invalid and returned for correction.
9
Other Group Plan Conditional Requirements and Attachments
If 'Other group plan drug coverage' is Yes, validates that the other insurer name, other plan contract number, other certificate number, and whether the drug is covered under the other plan are completed. If the drug is not covered under the other plan, the decline reason must be provided and a decline notice attachment should be present; if previously covered, proof of payment/EOB should be attached. If any conditional fields/attachments are missing, the request should be pended because coordination of benefits and eligibility for Manulife consideration cannot be confirmed.
10
Provincial Program Application/Decision Logic and Required Reasons
Validates that if provincial application is marked No, a reason is provided; and if provincial approval is marked No, a decline reason is provided. This is important because the plan may require provincial coverage to be pursued first and needs documentation to assess supplemental coverage. If missing, the submission should be pended until the reason (and any required provincial decision documentation, where applicable) is supplied.
11
Patient Assistance Program (PAP) Enrollment Conditional Details
If PAP enrollment is Yes, checks that case manager first/last name, phone, email, program name, and program ID are provided and properly formatted (phone/email rules applied). These details enable coordination and verification of support programs that may affect coverage and cost-sharing. If incomplete, the submission should be pended because follow-up and coordination may be delayed.
12
Treatment Administration Location Selection and Facility Details When Not Home
Validates that exactly one treatment administration location is selected (Home, MD office, Private Clinic, Hospital In-Patient, Hospital Out-patient). If the location is not Home, requires clinic/hospital name, telephone, and full address (street, city, province, postal code) to be completed; if MD office is in a hospital, requires the description field. If these are missing, the submission should be pended because site-of-care impacts assessment, billing, and coordination.
13
Drug Strength and Dosage Completeness and Dose Limit Consistency
Checks that Drug Strength and Dosage is populated with a meaningful regimen (strength and frequency at minimum) and is consistent with the 'Will dose of Wegovy exceed 2.4mg once weekly?' response. This prevents unclear prescriptions and ensures the request aligns with plan criteria and product labeling constraints used in prior authorization rules. If missing or contradictory (e.g., dosage indicates >2.4 mg weekly but checkbox says No), the submission should be pended for physician clarification.
14
Diagnosis Selection Required and Single-Path Completion
Validates that at least one diagnosis pathway is selected (pediatric initial/renewal, adult initial/renewal, MI risk reduction initial/renewal, or Any Other Diagnosis) and that the form is not completed across conflicting pathways simultaneously. Each pathway drives different clinical criteria and required fields, so mixing them can cause incorrect decisions. If no pathway is selected or multiple incompatible pathways are selected, the submission should be rejected/pended for correction.
15
Baseline Measurements Numeric Validation (Weight and BMI) and Plausibility
Ensures baseline body weight and BMI fields (where required by the selected pathway) are numeric, include reasonable decimal precision, and fall within plausible human ranges (with configurable thresholds). Accurate measurements are essential for eligibility (e.g., BMI thresholds, percent weight loss) and clinical appropriateness. If non-numeric, missing, or implausible, the submission should be pended and the prescriber asked to correct the values.
16
Adult Initial Comorbidity Dependency and 'Other' Specification
If 'weight-related comorbid condition present' is Yes, validates that at least one comorbidity checkbox is selected; if 'Other' is selected, the free-text other condition must be provided. This ensures the clinical rationale for therapy is documented and supports consistent adjudication. If comorbidity details are missing, the submission should be pended because eligibility criteria may not be met or cannot be verified.
17
Drug History Table Date Format/Order and Outcome Completeness
Validates that each entered prior/current therapy row has a drug name, start date and end date in yyyy/mmm format, and that end date is not earlier than start date (or is blank only if clearly indicated as ongoing per business rules). Also checks that at least one outcome (Intolerance or Inadequate/Suboptimal Response) is selected for each completed row, and that the 'continuing medication' Yes/No is answered. If incomplete or inconsistent, the submission should be pended because step-therapy/previous trial requirements cannot be assessed.
18
No Previous Therapies Rationale Required When Drug History Is Empty
If no drug therapy entries are provided in the drug history section, validates that at least one rationale checkbox (risk of interaction/contraindication/other) is selected and that the medical rationale narrative is completed. This prevents missing clinical justification when prior therapies have not been attempted. If absent, the submission should be rejected or pended because the prior authorization criteria often depend on documented prior therapy attempts or valid exceptions.
19
Physician Identity, License, and Contact Information Completeness
Ensures prescribing physician first/last name, college/license number, specialty, address, and telephone/fax are provided and formatted appropriately (phone/fax numeric formats; license number non-empty and pattern-checked if jurisdiction rules exist). This is required for verification, follow-up, and auditability of the medical attestation. If missing, the submission should be pended because the request cannot be validated as prescriber-authorized.
20
Signature and Signature Date Presence and Chronology (Physician and Plan Member)
Validates that both Physician Signature and Plan Member Signature are present, and that their corresponding dates are provided in dd/mmm/yyyy format and are not in the future. Optionally checks chronology (e.g., physician signature date should not be after plan member signature date by an unreasonable margin, or vice versa per business policy). If signatures/dates are missing or invalid, the submission must be rejected because consent and medical certification are legally required for processing.
Common Mistakes in Completing GL5197E (Wegovy)
This form uses multiple strict date formats (e.g., dd/mmm/yyyy for dates of birth and signatures, and yyyy/mmm for drug history start/end dates). People often enter numeric-only dates (e.g., 01/02/2026), use the wrong order (mm/dd), or write full month names, which can cause processing delays or requests for clarification. Always follow the exact format shown beside each field and keep it consistent across the form. AI-powered form filling tools like Instafill.ai can help by automatically formatting dates correctly and flagging mismatches before submission.
Plan contract number and plan member certificate number are frequently left blank, transposed, or copied from the wrong plan (especially when there is other coverage). If these identifiers don’t match Manulife’s records, the request may be delayed, misrouted, or rejected as “unable to locate member.” Use the numbers exactly as shown on the benefits card/plan documents and double-check for swapped digits. Instafill.ai can reduce errors by validating expected identifier formats and ensuring the right values populate the right fields.
When the patient is a spouse or dependent, people often enter the plan member’s details in the patient section (or vice versa), especially for name, date of birth, and contact information. This can lead to eligibility issues, incorrect clinical assessment, and delays because the medical criteria must match the actual patient. Confirm who is the plan member (coverage holder) and who is the patient (person taking Wegovy), and complete both sections fully when they are different. Instafill.ai can help by mapping identities consistently across fields and preventing accidental duplication.
Section 4 requires the prescriber to check the specific diagnosis/criteria pathway, but submissions often leave all diagnosis boxes unchecked or check multiple conflicting pathways. Without a clear pathway, Manulife can’t apply the correct eligibility criteria, which commonly triggers follow-up requests. Ensure exactly one appropriate section is selected (e.g., adult initial vs adult renewal) and that the answers provided correspond to that section. Instafill.ai can prompt for the required diagnosis selection and warn when answers don’t align with the chosen pathway.
Baseline body weight and BMI fields are often left blank, entered with unclear units, or inconsistent with the BMI threshold questions (e.g., BMI marked ≥30 but BMI value entered as 28). These values are central to approval criteria, so missing or inconsistent entries can result in denial or delays. Enter the numeric values clearly and ensure they support the checked eligibility answers; include units where helpful (kg and kg/m²). Instafill.ai can help by checking for internal consistency (e.g., BMI value vs. BMI threshold checkbox) and prompting for missing measurements.
The form asks whether Wegovy will be used with other GLP-1 analogs and whether the dose will exceed 2.4 mg once weekly; people sometimes answer based on past therapy, misunderstand what counts as a GLP-1, or leave these unchecked. Inconsistent or unsafe combinations/dosing can lead to denial or a request for prescriber clarification. The prescriber should confirm the current medication list and intended titration plan, then answer these questions precisely. Instafill.ai can help by standardizing medication lists and flagging potential conflicts or missing yes/no selections.
Section 2 expects the member to apply to applicable provincial programs first when relevant, and in Ontario specifically requires submitting the EAP approval/denial if the drug is an EAP drug. People often check “No” without explaining why, or fail to attach the provincial decision letter, which can halt assessment under the Manulife plan. Provide the reason if no application was made, and attach the provincial approval/denial documentation when applicable. Instafill.ai can help by prompting for required attachments based on province and ensuring the “reason” fields are completed when “No” is selected.
When there is other group coverage, members frequently check “Yes” but omit the other insurer’s details, forget to indicate whether the drug is covered, or fail to attach the required decline notice/proof of payment. Manulife may need the other plan’s decline notice (and for renewals, a current one) to determine whether Manulife can approve coverage, so missing documents commonly cause delays. Complete all fields under 1A/1B when “Yes” is selected and attach the exact documents requested (decline letter/statement or receipt/EOB). Instafill.ai can guide conditional sections so the right follow-up fields and attachments are not missed.
Section 5 is often submitted with drug names only, without start/end dates (yyyy/mmm), without selecting an outcome (intolerance vs inadequate response), or without indicating whether the patient will continue the medication alongside Wegovy. Incomplete therapy history makes it difficult to assess medical necessity and can trigger requests for more information. The prescriber should list all relevant prior/current therapies, include approximate months/years if exact dates are unknown, and select the appropriate outcome and continuation status for each. Instafill.ai can help by enforcing required sub-fields per therapy line and formatting dates consistently.
People sometimes check a non-home administration site (MD office/clinic/hospital) but leave the clinic/hospital name, address, and phone blank, or they answer the “MD office located in a hospital” question inconsistently with the selected location. Missing site-of-care details can delay coordination and verification, especially when hospital/clinic administration is involved. If not administered at home, provide complete facility contact information and clarify where in the hospital/MD office the drug will be administered when asked. Instafill.ai can prevent this by requiring facility fields when “Home” is not selected and flagging contradictory selections.
A common rejection reason is missing the physician signature/date, missing the plan member signature/date, or submitting an older/modified version of the form (the form explicitly requests the most current unaltered version). Without valid signatures and dates, Manulife may not be able to legally process the authorization and medical information. Ensure both the prescriber and plan member sign and date in dd/mmm/yyyy, and download the latest form version from Manulife before completing it. If the form is only available as a flat non-fillable PDF, Instafill.ai can convert it into a fillable version and help ensure required signature/date fields are not overlooked.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out GL5197E (Wegovy) with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills manulife-group-benefits-drug-prior-authorization-form-wegovysemaglutide-gl5197e-mli-082025-wegov forms, ensuring each field is accurate.