Yes! You can use AI to fill out Shoulder and Arm Conditions Disability Benefits Questionnaire
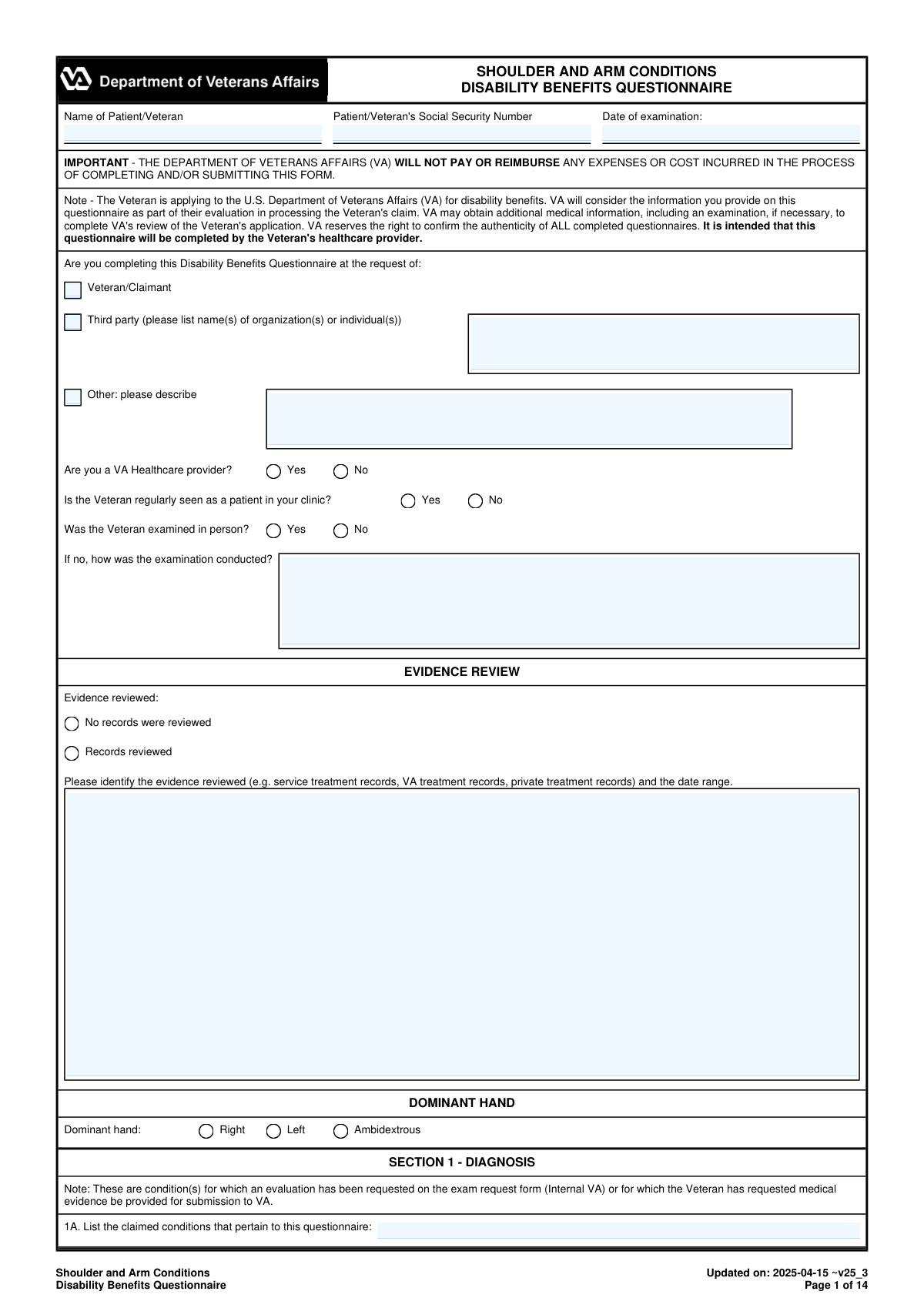
The Shoulder and Arm Conditions Disability Benefits Questionnaire (DBQ) is an official Department of Veterans Affairs medical evaluation form completed by a clinician to provide standardized evidence for VA disability compensation decisions. It captures key clinical details such as diagnoses (with ICD codes), dominant hand, medical history, range-of-motion testing (active/passive, weight-bearing/nonweight-bearing), flare-ups, repetitive-use limitations, and results of special tests and imaging. The DBQ is important because VA uses it to assess severity, functional impact, and service-connection-related medical evidence in a consistent format. Accurate, complete entries and examiner certification help reduce delays and improve the reliability of the claim evidence.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out VA DBQ (Shoulder and Arm Conditions) using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Shoulder and Arm Conditions Disability Benefits Questionnaire |
| Number of pages: | 14 |
| Language: | English |
| Categories: | VA forms, disability forms, veteran forms, medical assessment forms, veterans forms, medical disability forms, medical forms, benefit forms |
Instafill Demo: filling out a legal form in seconds
How to Fill Out VA DBQ (Shoulder and Arm Conditions) Online for Free in 2026
Are you looking to fill out a VA DBQ (SHOULDER AND ARM CONDITIONS) form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your VA DBQ (SHOULDER AND ARM CONDITIONS) form in just 37 seconds or less.
Follow these steps to fill out your VA DBQ (SHOULDER AND ARM CONDITIONS) form online using Instafill.ai:
- 1 Enter Veteran/patient identifiers and exam details (name, SSN, date of exam), and indicate who requested the DBQ and whether the exam was in-person or remote (and how conducted).
- 2 Complete the Evidence Review and Dominant Hand sections, listing records reviewed (types and date ranges) and selecting the Veteran’s dominant hand.
- 3 Document Section 1 (Diagnosis) by listing claimed conditions, selecting all applicable diagnoses, specifying side affected (right/left/both), and adding ICD codes and diagnosis dates; add any “other” diagnoses as needed.
- 4 Fill out Medical History (Section 2) including onset/course, flare-ups (frequency, duration, triggers, relief), and the Veteran’s reported functional loss after repeated use over time.
- 5 Record Range of Motion and functional limitation (Section 3) for each shoulder: active and passive ROM values, pain with motion (active/passive, weight-bearing/nonweight-bearing), repetitive-use testing results, and estimated ROM during repeated use over time and flare-ups with supporting rationale.
- 6 Complete remaining clinical sections as applicable (muscle atrophy, ankylosis, rotator cuff tests, instability/labral pathology, clavicle/scapula/AC joint issues, humerus impairments, surgeries, scars/other findings, assistive devices, remaining effective function, and diagnostic testing/imaging).
- 7 Describe Functional Impact (Section 15), add any Remarks (Section 16), then finalize with Examiner Certification and Signature (Section 17) including credentials, specialty, contact info, NPI, license details, and address before generating the final submission-ready form.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable VA DBQ (Shoulder and Arm Conditions) Form?
Speed
Complete your VA DBQ (Shoulder and Arm Conditions) in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 VA DBQ (Shoulder and Arm Conditions) form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form VA DBQ (Shoulder and Arm Conditions)
This DBQ documents a Veteran’s shoulder/arm diagnoses, symptoms, and functional limitations so VA can evaluate a disability benefits claim. VA uses the medical findings in this form as evidence when deciding the claim.
It is intended to be completed by the Veteran’s healthcare provider (examiner), not the Veteran. The examiner must certify and sign the form in Section 17.
Yes. The form asks whether the examiner is a VA healthcare provider, but private clinicians can complete it as long as they provide required credentials (e.g., license, NPI) and sign the certification.
No. The form states VA will not pay or reimburse any expenses or costs incurred to complete or submit the questionnaire.
Not always, but the form asks whether the Veteran was examined in person and, if not, how the exam was conducted. The examiner should document the method used and ensure the findings are supportable.
In the Evidence Review section, the examiner indicates whether records were reviewed and lists what was reviewed (e.g., service treatment records, VA records, private records) and the date range. If no records were reviewed, that must be checked.
Dominant hand (right/left/ambidextrous) can affect how VA evaluates functional impact and severity, especially when the condition affects the dominant upper extremity.
The examiner can select that there is no current diagnosis associated with the claimed conditions and must explain the findings and reasoning in the Remarks section. VA may still consider symptoms, but clear medical explanation is important.
In Section 1B, each diagnosis includes a “Side affected” choice (Right/Left/Both) and space for ICD code and date of diagnosis. Be consistent with the history and exam findings throughout the form.
The form requests active ROM and passive ROM values for flexion, abduction, internal rotation, and external rotation (in degrees), and asks which movements show pain. It also asks for pain on active vs. passive motion and weight-bearing vs. nonweight-bearing when possible.
The examiner should mark “Unable to test” or indicate testing cannot be performed and provide a clear medical explanation in the space provided. The form specifically requires an explanation when testing is not done or is medically contraindicated.
Sections 3C and 3D ask the examiner to use “procured evidence,” including the Veteran’s statements and available records, to estimate additional functional loss and ROM during repeated use over time and flare-ups. If an estimate cannot be provided, the examiner must explain why based on case-specific evidence (not simply because it wasn’t observed).
Section 3B asks whether the Veteran can perform at least three repetitions and whether ROM decreases afterward. If there is additional loss, the examiner records the post-test ROM values and identifies contributing factors (pain, weakness, fatigability, etc.).
Imaging is not required for every condition, but degenerative or post-traumatic arthritis must be confirmed by imaging. If arthritis has already been documented in the past, VA does not require new imaging solely to confirm it again.
The examiner must sign and date the form and provide printed name/title, specialty, phone/fax, NPI number, medical license number and state, and address. The certification also warns of penalties for knowingly submitting false statements.
Compliance VA DBQ (Shoulder and Arm Conditions)
Validation Checks by Instafill.ai
1
Patient/Veteran Identifiers Present and Properly Formatted
Validates that the Patient/Veteran name and Social Security Number (SSN) fields are not blank and that the SSN is exactly 9 digits (optionally allowing standard hyphen formatting XXX-XX-XXXX). These identifiers are required to correctly associate the DBQ with the correct claimant and prevent misfiling. If validation fails, the submission should be rejected or routed to an exception queue for manual resolution before it can be used for a claim decision.
2
Examination Date and Signature Date Validity
Checks that 'Date of examination' and 'Date Signed' are present, are valid calendar dates, and follow the expected format (e.g., YYYY-MM-DD or MM/DD/YYYY per system standard). It also verifies that the signature date is on or after the examination date and not in the future. If invalid or inconsistent, the form should be flagged because it undermines the legal/clinical timeliness and authenticity of the report.
3
Requestor Type Selection and Conditional Third-Party Details
Ensures exactly one requestor type is selected (Veteran/Claimant, Third party, or Other). If 'Third party' is selected, at least one organization/individual name must be provided; if 'Other' is selected, a description must be provided. If this validation fails, the submission should be returned for completion because the provenance of the DBQ request affects auditability and potential conflicts of interest.
4
Provider Status and Clinic Relationship Consistency
Validates that 'Are you a VA Healthcare provider?' and 'Is the Veteran regularly seen as a patient in your clinic?' are answered and are logically consistent with the context of the exam. For example, if the provider indicates they are not a VA provider but the system requires VA-only submissions for a workflow, it should be flagged; similarly, missing answers reduce credibility and completeness. Failures should trigger a completeness error and require correction before acceptance.
5
In-Person Exam Requirement and Remote Exam Explanation
Checks that 'Was the Veteran examined in person?' is answered, and if 'No' is selected, the method of examination (telehealth, records review, etc.) is provided in the follow-up field. This is important because VA adjudication may weigh in-person objective findings differently than remote assessments. If missing, the form should be marked incomplete and prevented from final submission.
6
Evidence Review Selection and Required Evidence Details
Ensures the evidence review section is internally consistent: either 'No records were reviewed' is selected, or 'Records reviewed' is selected with a non-empty description of evidence types and a date range. If records were reviewed, the date range must be parseable (start and end dates) and the start date must be on/before the end date. If validation fails, the submission should be flagged because the basis for medical opinions and estimates (e.g., flare-up ROM estimates) becomes unclear.
7
Dominant Hand Selection Required
Validates that exactly one dominant hand option is selected (Right, Left, or Ambidextrous). Dominance can affect functional impact and interpretation of impairment severity. If missing or multiple selections occur, the form should be rejected for correction to avoid downstream rating inconsistencies.
8
Diagnosis Selection Requires Side, ICD Code, and Diagnosis Date
For each checked diagnosis in Section 1B, validates that a side affected (Right/Left/Both) is selected and that ICD code and date of diagnosis are provided in valid formats. If 'Both' is selected, the form should not simultaneously require separate right/left entries unless the template explicitly supports it; the system should enforce one consistent representation. Failures should block submission because diagnoses without laterality and coding are not actionable for claims processing and analytics.
9
No Current Diagnosis Requires Remarks Explanation
If the option 'The Veteran does not have a current diagnosis associated with any claimed conditions listed above' is selected, the remarks section must include an explanation of findings and reasons. This prevents a clinically empty record and supports adjudicators in understanding why claimed conditions were not diagnosed. If missing, the form should be returned as incomplete.
10
ROM Measurement Completeness When Testing Is Performed
When ROM testing is indicated as performed for a shoulder, validates that active ROM values (flexion, abduction, internal rotation, external rotation) are all present and numeric. It also checks that passive ROM is either fully populated with numeric values or explicitly marked 'Same as active ROM' for each movement. If incomplete, the submission should be flagged because VA rating criteria rely heavily on complete ROM data.
11
ROM Numeric Range and Unit Validation
Validates that ROM degree entries are numeric and within physiologically plausible bounds: flexion/abduction 0–180 and internal/external rotation 0–90, with no negative values. It also ensures the unit is degrees (not text like 'full' or 'WNL') and that endpoints are not left blank when required. If out of range or non-numeric, the system should reject the entry or require correction to prevent erroneous disability evaluations.
12
Unable/Not Indicated ROM Requires Explanation
If 'Unable to test' or 'Not indicated' is selected for initial ROM measurements, an explanation must be provided in the corresponding text field. This is required to document medical contraindications, severe pain, or other barriers to testing. If missing, the form should be considered incomplete because it prevents reviewers from determining whether missing ROM is justified.
13
Pain Evidence and Functional Loss Consistency
If 'Is there evidence of pain?' is marked 'Yes', at least one applicable context (weight-bearing, nonweight-bearing, active, passive, rest) should be selected, and if 'causes functional loss' is checked, a comment describing how it causes functional loss must be present. Conversely, if pain is 'No', pain context checkboxes should not be selected. Failures should be flagged because pain-related functional loss is a key component of VA musculoskeletal evaluations.
14
Repetitive-Use Testing Logic and Required Follow-Ups
Validates that if the Veteran is able to perform repetitive-use testing, the form records whether there is additional loss after three repetitions; if 'Yes', the post-test ROM values and at least one causative factor (pain, fatigability, weakness, lack of endurance, incoordination, other) must be selected. If the Veteran is not able to perform repetitive-use testing, an explanation is required. If validation fails, the submission should be held because repetitive-use findings are required for accurate functional assessment.
15
Repeated Use Over Time / Flare-Up Estimates or Feasibility Explanation
When procured evidence suggests significant limitation with repeated use over time or flare-ups, the estimated ROM fields should be completed with numeric degree values; if the examiner states it is not feasible to estimate, a case-specific explanation and cited evidence must be provided. This enforces the DBQ instruction that estimates should be attempted based on all procurable information. If missing, the form should be flagged for correction because it may be noncompliant with required VA examination standards.
16
Examiner Credentialing and Contact Information Format Validation
Validates that the examiner signature, printed name/title, specialty, NPI, license number/state, address, and phone/fax are present and properly formatted (NPI as 10 digits; phone/fax as valid 10-digit US numbers with optional punctuation; license state as a valid US state/territory code). These fields support authenticity verification and allow VA to contact the examiner for clarification. If validation fails, the submission should be rejected or routed for manual verification due to high fraud/identity risk.
Common Mistakes in Completing VA DBQ (Shoulder and Arm Conditions)
People often leave the header fields blank or enter identifiers inconsistently across pages because they focus on the clinical sections first. Missing SSN, patient name, or the date of examination can cause the DBQ to be rejected, misfiled, or delayed while VA requests clarification. Always complete the top identifiers exactly as they appear in the Veteran’s records and ensure the exam date reflects when the evaluation occurred (not when the form is submitted).
The “at the request of” question is frequently skipped or multiple options are checked without listing the organization/person. This creates ambiguity about the purpose and provenance of the report and can trigger follow-up requests to verify authenticity. Check only one option and, if “Third party” or “Other,” clearly list the requesting entity and a brief description.
A common error is marking “Was the Veteran examined in person? No” but leaving the “If no, how was the examination conducted?” blank, or providing a vague answer like “telehealth” without details. VA often needs to understand the limitations of a non-in-person exam to weigh findings appropriately. If not in person, specify the method (video/phone/records review), what was and wasn’t assessed, and why in-person testing was not performed.
Clinicians often check “Records reviewed” but fail to identify which records and the date range, or they check “No records were reviewed” even though they reference imaging later. This undermines credibility and can lead VA to discount opinions that should be supported by records. List the specific sources (e.g., STRs, VA treatment records, private ortho notes, imaging reports) and include an approximate date range that matches what you actually reviewed.
Dominant hand is frequently omitted or marked incorrectly, especially when both shoulders are involved. Dominance can affect functional impact and rating considerations, and inconsistencies can raise questions about accuracy. Confirm dominance directly with the Veteran and ensure later “side affected” and functional impact narratives align with that dominance.
It’s common to accidentally check “The Veteran does not have a current diagnosis…” and still select diagnoses below, or to list a condition without side, ICD code, or date of diagnosis. These contradictions can cause VA to treat the DBQ as internally inconsistent and request a new exam. Only check the “no diagnosis” box if truly applicable, and for each diagnosis provide side affected, ICD code when available, and a defensible diagnosis date (initial diagnosis date or approximate based on records/history).
People often mark “Both” but then provide ROM or test results for only one shoulder, or they document arm symptoms without tying them to the correct shoulder side. This leads to unclear attribution of limitations and can affect how VA rates each extremity. For every relevant section (ROM, tests, atrophy, instability), ensure right and left are completed separately and that narratives explicitly reference the correct side.
A frequent data-entry issue is leaving ROM endpoints blank, writing qualitative terms (“limited,” “normal”), or entering values that exceed the stated normals (e.g., flexion >180 or rotation >90). VA requires numeric degree measurements to apply rating criteria, and implausible values can invalidate the exam. Record active and passive ROM in degrees using a goniometer when possible, keep values within physiologic limits, and use “Same as active ROM” only when truly identical and documented.
Examiners often document “pain present” but fail to indicate whether pain occurs on active vs passive motion and weight-bearing vs nonweight-bearing, or they skip the “Can testing be performed?” explanations. VA guidance expects these contexts (or a medical rationale for why they can’t be tested), and missing details can prompt remand or re-exam. Explicitly check the applicable pain contexts and, if any testing is not performed, provide a case-specific medical reason (e.g., risk of injury, severe pain).
A very common mistake is answering that repeated use/flare-ups significantly limit function but leaving the estimated ROM during repeated use or flare-ups blank, or stating “unable to estimate without observing” without a case-specific explanation. VA expects an estimate based on procurable information (Veteran statements, records, clinical judgment), and generic refusals can make the DBQ inadequate. Provide best medical estimates in degrees when possible and, if not feasible, explain specifically what information is missing and why it prevents an estimate in this particular case.
People often check that surgery or imaging occurred but omit the date, type of procedure/test, side, and a brief results summary, or they claim degenerative arthritis without imaging confirmation. This can weaken the evidentiary basis for diagnoses like osteoarthritis and delay adjudication while VA seeks records. Include procedure/test type, approximate date, side(s), and key findings (e.g., MRI tear, X-ray OA changes), and only mark arthritis as documented if imaging supports it.
DBQs are frequently returned because the examiner forgets to sign, omits credentials/title, leaves NPI or license/state blank, or provides an incomplete address/phone. VA may question authenticity or be unable to verify the provider, which can invalidate the submission. Complete every field in Section 17, ensure the signature and date signed are present, and verify that NPI and license information match the examiner’s official records.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out VA DBQ (Shoulder and Arm Conditions) with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills shoulder-and-arm-conditions-disability-benefits-qu forms, ensuring each field is accurate.