Yes! You can use AI to fill out 1199SEIU Benefit Funds Applied Behavior Analysis (ABA) Prior Authorization Form
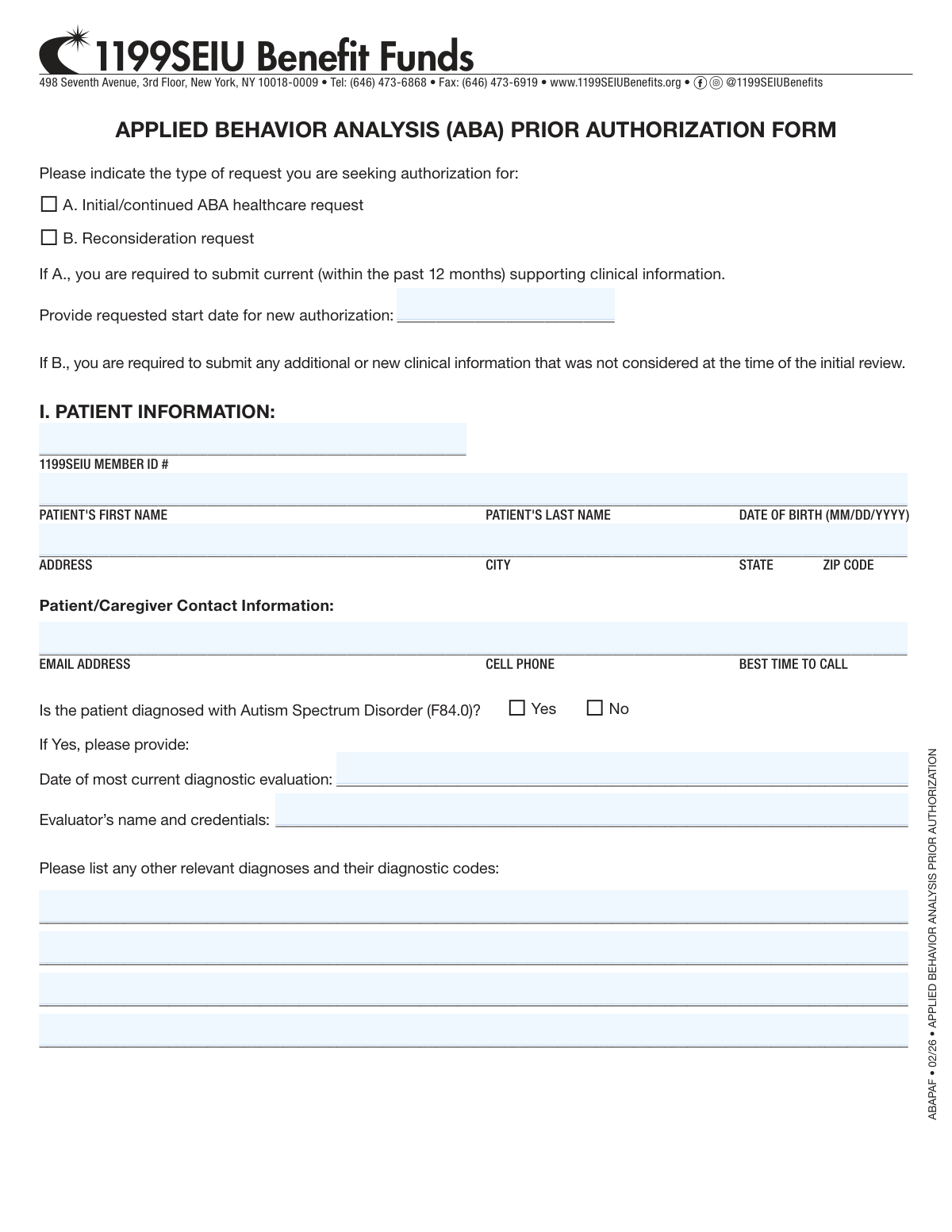
The 1199SEIU Applied Behavior Analysis (ABA) Prior Authorization Form (ABAPAF) is an official document required by the 1199SEIU Benefit Funds to authorize ABA therapy services for members diagnosed with Autism Spectrum Disorder or other qualifying conditions. It captures detailed patient information, provider credentials, requested service codes and units, treatment settings, and supporting clinical documentation to facilitate the review and approval process. Submitting this form accurately is critical to ensuring timely access to ABA therapy without interruption in care. Today, this form can be filled out quickly and accurately using AI-powered services like Instafill.ai, which can also convert non-fillable PDF versions into interactive fillable forms.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out ABAPAF using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | 1199SEIU Benefit Funds Applied Behavior Analysis (ABA) Prior Authorization Form |
| Number of pages: | 3 |
| Language: | English |
Instafill Demo: filling out a legal form in seconds
How to Fill Out ABAPAF Online for Free in 2026
Are you looking to fill out a ABAPAF form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your ABAPAF form in just 37 seconds or less.
Follow these steps to fill out your ABAPAF form online using Instafill.ai:
- 1 Navigate to Instafill.ai and upload the ABAPAF form PDF or select it from the available form library to begin filling it out online.
- 2 Indicate the type of request (Initial/Continued ABA healthcare request or Reconsideration request) and provide the requested authorization start date if applicable.
- 3 Complete Section I – Patient Information, including the 1199SEIU Member ID, patient name, date of birth, address, contact details, ASD diagnosis status, diagnostic evaluation date, evaluator credentials, and any other relevant diagnoses.
- 4 Complete Section II – Provider Information, entering the clinic name, address, tax ID, NPI, phone, fax, email, supervising provider's name and credentials, and details about any additional supervision providers.
- 5 Enter the requested ABA service units and hours for each applicable CPT/procedure code (97151, 97152, 97153–97158, 0373T, 0362T), specifying frequency (per week or per month) and total units for the authorization period.
- 6 Select the ABA treatment place(s) of service, indicate any additional services the patient is receiving, and document the standardized assessments administered along with current, baseline, and previous scores.
- 7 Review all entered information for accuracy, then have the authorized provider print their name, enter their title, sign, and date the form before submitting it to 1199SEIU Benefit Funds via fax or the designated submission method.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable ABAPAF Form?
Speed
Complete your ABAPAF in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 ABAPAF form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form ABAPAF
This form is used to request prior authorization for Applied Behavior Analysis (ABA) therapy services through 1199SEIU Benefit Funds. It covers both initial/continued ABA healthcare requests and reconsideration requests for members whose previous authorization was denied or requires review.
This form must be completed by the ABA provider or clinic on behalf of a 1199SEIU member (or their dependent) who requires ABA therapy services. The supervising provider, such as a BCBA or licensed psychologist, is responsible for completing and signing the form.
An Initial/Continued ABA request (Option A) is for new or ongoing ABA therapy authorization and requires current clinical information from within the past 12 months. A Reconsideration request (Option B) is used when a previous authorization was denied, and it requires submission of any additional or new clinical information that was not considered during the initial review.
For an initial or continued request, you must submit current supporting clinical information dated within the past 12 months, including diagnostic evaluation records confirming an Autism Spectrum Disorder (ASD) diagnosis (ICD-10 code F84.0). For a reconsideration request, you must include any new or additional clinical information not previously reviewed.
Yes, the form specifically asks whether the patient has been diagnosed with Autism Spectrum Disorder (F84.0). If yes, you must provide the date of the most recent diagnostic evaluation and the evaluator's name and credentials. Other relevant diagnoses and their codes should also be listed.
The supervising provider must be credentialed or licensed as a BCBA, BCBA-D, LBA, Licensed Psychologist, or another specified credential. If multiple providers are involved in supervision, all of their names and credentials must be listed on the form.
The form includes ABA assessment codes (97151, 97152), BCBA/supervision codes (97155, 97156, 97157, 97158, 0373T, 0362T), and technician/RBT codes (97153, 97154). For each code, you must specify the number of units, hours, frequency (per week or per month), and total units for the authorization period.
ABA services can be provided in a clinic, home, school, community setting, virtually, or in-person. You must check all applicable settings on the form to ensure the authorization covers all locations where treatment will be delivered.
You must indicate which standardized assessments were administered, including the name of the assessment, the date it was administered, and the current, baseline, and previous scores. If this information is included in the treatment plan, you may reference the relevant page numbers instead.
Completed forms can be submitted by fax to (646) 473-6919 or by mail to 498 Seventh Avenue, 3rd Floor, New York, NY 10018-0009. You can also visit www.1199SEIUBenefits.org for additional submission options and information.
Yes, AI-powered services like Instafill.ai can help you accurately auto-fill form fields, saving time and reducing errors. These tools are especially useful for complex forms like this one that require detailed clinical and provider information.
You can upload the ABA Prior Authorization Form to Instafill.ai, where the AI will guide you through each field and auto-fill information accurately based on your inputs. This makes the process faster and helps ensure all required sections are completed correctly before submission.
If you have a flat, non-fillable PDF version of this form, Instafill.ai can convert it into an interactive fillable form so you can type directly into the fields. This eliminates the need to print and handwrite the form, making the process more efficient.
If the patient is receiving any additional services alongside ABA therapy, you must check all that apply, including Mental Health Services, Speech Therapy, Occupational Therapy, Physical Therapy, School System Services, Primary Care (Pediatrician), Medication Management, or any other treatment. This helps the reviewer understand the full scope of the patient's care.
You must provide the patient's 1199SEIU Member ID, first and last name, date of birth, full address, email address, cell phone number, and best time to contact. This information ensures the authorization request is correctly linked to the member's account.
Compliance ABAPAF
Validation Checks by Instafill.ai
1
Request Type Selection is Required
The form must have exactly one request type selected: either 'A. Initial/continued ABA healthcare request' or 'B. Reconsideration request.' This selection drives downstream requirements, such as whether current clinical information or new/additional clinical information must be submitted. If neither or both options are selected, the form cannot be properly routed or reviewed, and the submission should be rejected with a request to clarify the intent.
2
Requested Start Date is Required for Initial/Continued Requests
When request type 'A' (Initial/continued ABA healthcare request) is selected, the requested start date field must be populated with a valid date in MM/DD/YYYY format. This date is critical for scheduling the authorization period and ensuring timely service delivery. If the start date is missing or improperly formatted, the authorization period cannot be established, and the request must be returned to the submitter.
3
1199SEIU Member ID Format and Presence Validation
The 1199SEIU Member ID field is required and must conform to the expected alphanumeric format used by the 1199SEIU Benefit Funds. An invalid or missing Member ID prevents the system from linking the prior authorization request to an active member account and verifying eligibility. Submissions with a blank or incorrectly formatted Member ID must be flagged and returned before any clinical review can begin.
4
Patient Date of Birth Format and Logical Range Check
The patient's date of birth must be entered in MM/DD/YYYY format and must represent a valid calendar date. Additionally, the date of birth should reflect a plausible age for an ABA patient (typically a minor or young adult), and the date must not be in the future. An invalid or future date of birth indicates a data entry error that could result in misidentification of the patient or incorrect eligibility determination.
5
Autism Spectrum Disorder Diagnosis Confirmation is Required
The form requires a definitive Yes or No answer to whether the patient has been diagnosed with Autism Spectrum Disorder (ICD-10 code F84.0). ABA therapy prior authorization is specifically tied to this diagnosis, and an unanswered question creates ambiguity about medical necessity. If 'Yes' is selected, the date of the most current diagnostic evaluation and the evaluator's name and credentials must also be provided; if these dependent fields are missing, the form is incomplete.
6
Diagnostic Evaluation Date Must Be Within a Clinically Reasonable Timeframe
When the patient is confirmed to have an ASD diagnosis, the date of the most current diagnostic evaluation must be provided in a valid date format and should be reviewed for clinical recency. While the form does not specify a hard cutoff for the diagnostic evaluation date (unlike the 12-month requirement for clinical information), an evaluation date that is implausibly old or in the future should be flagged for reviewer attention. Missing this date when ASD is confirmed leaves the authorization without a documented diagnostic basis.
7
Provider NPI Number Format Validation
Both the clinic/facility NPI and the individual supervising provider's NPI must be present and must conform to the standard 10-digit National Provider Identifier format as defined by CMS. An invalid NPI prevents verification of the provider's enrollment status and credentialing with the benefit fund. Submissions containing NPIs that are fewer or greater than 10 digits, or that contain non-numeric characters, must be rejected and corrected before processing.
8
Facility Tax ID Format Validation
The Facility Tax ID (EIN) must be present and formatted as a 9-digit number, typically in the XX-XXXXXXX format. This identifier is required to process claims and verify the billing entity associated with the authorization request. A missing or incorrectly formatted Tax ID will prevent the fund from associating the authorization with a recognized and credentialed provider organization.
9
Supervising Provider Credential Selection is Required
At least one credential must be selected for the individual supervising provider from the options: BCBA, BCBA-D, LBA, Licensed Psychologist, or Other. ABA services must be supervised by a qualified professional, and the credential type determines the scope of permissible supervision activities under the plan's coverage policies. If 'Other' is selected, the free-text specification field must also be populated; an empty credential section or an 'Other' selection without specification renders the form incomplete.
10
Additional Supervision Disclosure When Primary Supervisor Does Not Provide All Supervision
If the answer to 'Is the provider above providing all supervision for the patient's ABA treatment?' is 'No,' then the fields listing additional supervisors and their credentials must be completed. Incomplete disclosure of all supervising providers creates a gap in the clinical oversight record and may result in services being rendered by unverified personnel. The form should be returned if the 'No' option is selected but the additional supervisor fields are left blank.
11
At Least One CPT Code Unit Request Must Be Populated
The form includes multiple ABA-specific CPT codes (97151, 97152, 97153, 97154, 97155, 97156, 97157, 97158, 0373T, 0362T), and at least one of these must have units, hours, and frequency (per week or per month) populated along with a total number of units for the authorization period. A form with no service units requested provides no basis for authorization and cannot be reviewed for medical necessity. Each populated CPT code row must have internally consistent values where the total units per authorization period align with the stated weekly or monthly frequency.
12
Per Week or Per Month Frequency Must Be Exclusively Selected for Each CPT Code
For each CPT code row where units are requested, exactly one frequency option—either 'per week' or 'per month'—must be selected, not both and not neither. Selecting both or neither makes it impossible to calculate the total authorized units over the authorization period and introduces ambiguity into the service plan. Any CPT code row with units entered but no frequency selection, or with both frequency options checked, must be flagged as an error requiring correction.
13
Place of Service Selection is Required
At least one ABA treatment place of service must be selected from the available options: Clinic, Home, School, Community, Virtual, or In-person. The place of service affects coverage determination, rate setting, and coordination of care requirements under the benefit plan. A form submitted without any place of service indicated is missing a key clinical and administrative data point and must be returned for completion.
14
Form Completion Date Must Be Valid and Not in the Future
The 'DATE (MM/DD/YYYY)' field at the bottom of the form must be populated with a valid date in the correct format and must not be a future date. The completion date establishes the timeliness of the submission relative to the requested start date and any applicable filing deadlines. A missing, improperly formatted, or future completion date undermines the integrity of the submission record and may affect whether the request is considered timely.
15
Signature Field Must Be Completed by the Form Completer
The signature field associated with the 'Form completed by' section must be signed, and the corresponding PRINT NAME and TITLE fields must also be populated. An unsigned or incomplete attestation section means there is no accountable party for the clinical information submitted, which is a requirement for prior authorization submissions under most benefit plan policies. Forms lacking a signature, printed name, or title must be returned as incomplete before any clinical review is initiated.
16
Standardized Assessment Information Must Be Provided with Current, Baseline, and Previous Scores
The standardized assessment section requires the name of the assessment, the date it was administered, and at minimum a current score to support the medical necessity determination. For continued authorization requests, baseline and previous scores are also critical to demonstrate treatment progress or lack thereof. If the assessment name and date are provided but scores are entirely absent, or if the section is completely blank with no reference to page numbers in the treatment plan, the clinical justification for the requested services is insufficient and the form should be flagged for follow-up.
Common Mistakes in Completing ABAPAF
Many applicants overlook or misunderstand the distinction between an Initial/Continued ABA request (Option A) and a Reconsideration request (Option B), sometimes selecting the wrong one or leaving it blank entirely. This causes delays because each type requires different supporting documentation — Option A requires clinical information from within the past 12 months, while Option B requires new or additional information not previously considered. Submitting the wrong type can result in outright rejection or a request for resubmission. Carefully read both options before selecting, and ensure your attached documentation matches the requirements of the type you choose.
The Member ID is a critical identifier that links the patient to their benefits plan, and applicants frequently enter it incorrectly, transpose digits, or leave it blank. Without a valid Member ID, the form cannot be processed and will be returned, causing significant delays in authorization. Always double-check the Member ID against the physical membership card or benefits portal before submitting. AI-powered form filling tools like Instafill.ai can help by auto-populating and validating member ID formats to reduce transcription errors.
The form explicitly requires dates in MM/DD/YYYY format, but applicants frequently enter dates in other formats such as MM/DD/YY, YYYY-MM-DD, or written out (e.g., 'March 5, 2010'). Inconsistent date formatting can cause processing errors or mismatches in the system, potentially delaying or invalidating the authorization request. Always verify that every date field — including Date of Birth, diagnostic evaluation date, and the form completion date — follows the MM/DD/YYYY format exactly. Tools like Instafill.ai automatically enforce correct date formatting to prevent this common error.
For Initial/Continued requests, the form requires current clinical information from within the past 12 months, yet many submitters attach older evaluations or fail to provide the date of the most recent diagnostic evaluation. Submitting outdated documentation is one of the most common reasons for prior authorization denial, as it does not reflect the patient's current clinical status. Ensure the diagnostic evaluation date is within the required 12-month window and that the evaluator's name and credentials are fully and accurately listed. Review all attached documents for their dates before submission.
Applicants often leave the Individual Supervising Provider's Tax ID, NPI number, or credential checkboxes (BCBA, BCBA-D, LBA, Licensed Psychologist, Other) incomplete or inaccurate. Missing or incorrect NPI and Tax ID numbers can prevent the claim from being matched to a credentialed provider in the system, resulting in denial. Ensure all provider identifiers are verified against official records, and check all applicable credential boxes — if 'Other' is selected, the specific credential must be written in. Instafill.ai can help validate NPI number formats and flag missing required fields before submission.
The form requires detailed unit and hour breakdowns for multiple CPT codes (97151, 97152, 97153, 97154, 97155, 97156, 97157, 97158, 0373T, 0362T), including per-week or per-month frequency and total units for the authorization period. A very common mistake is entering inconsistent numbers — for example, units per week that don't mathematically align with the total units per authorization period, or confusing 'units' with 'hours.' These discrepancies raise red flags during review and can lead to denial or requests for clarification. Double-check all arithmetic and ensure the per-week/per-month selection is clearly indicated for each code.
Each CPT code section requires the submitter to specify whether the units and hours listed are per week or per month, but this checkbox is frequently left blank or inconsistently filled. Leaving the frequency unspecified makes it impossible for reviewers to accurately assess the scope of services being requested, which can result in the form being returned or the authorization being denied. Review every service code row and confirm that either 'per week' or 'per month' is clearly selected for each one. This is especially easy to miss on a complex multi-code form like this one.
When the supervising provider is not solely responsible for all ABA supervision (i.e., 'No' is selected for the supervision question), the form requires a complete list of all other supervising individuals and their credentials. Many submitters select 'No' but then leave the follow-up fields blank, which creates an incomplete record and may raise compliance concerns during review. If multiple supervisors are involved, list each one with their full name and credentials in the provided lines. Incomplete supervision disclosure can delay authorization or trigger additional information requests.
The form requires the name and date of each standardized assessment administered, along with current, baseline, and previous scores. Applicants frequently leave these fields blank, provide only partial scores, or fail to reference the correct page numbers in the treatment plan where this information can be found. Missing assessment data weakens the clinical justification for the requested services and is a common reason for denial. Ensure all three score fields (Current, Baseline, Previous) are completed for each assessment, and if referencing a treatment plan, clearly note the exact page numbers.
The form asks providers to check all applicable places of service (Clinic, Home, School, Community, Virtual, In-person), but this section is often skipped or only partially completed. Failing to indicate where services will be delivered can result in authorization being granted for a narrower scope than intended, causing billing issues later. Review all locations where ABA services will be provided and check every applicable box. Remember that multiple locations can and should be selected if the patient receives services in more than one setting.
The form requires a printed name, title, signature, and date from the person completing it, yet these fields are frequently left blank, signed but undated, or completed with an illegible signature without a printed name. An unsigned or improperly completed form is considered invalid and will not be processed, causing significant delays in the authorization timeline. Ensure all four fields — printed name, title, signature, and date in MM/DD/YYYY format — are fully and legibly completed before submission. If submitting electronically, confirm that the e-signature fields are properly executed.
The form itself is only one component of the prior authorization request — for Initial/Continued requests, current clinical documentation (within the past 12 months) must be submitted alongside the form, and for Reconsideration requests, new or additional clinical information is required. A very common mistake is submitting the completed form without the necessary attachments, or attaching documents that are outdated or irrelevant to the current request. Create a checklist of all required documents before submission and verify that each attachment is current, relevant, and clearly labeled. Instafill.ai can help prompt users to attach required supporting documents as part of the submission workflow.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out ABAPAF with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills 1199seiu-benefit-funds-applied-behavior-analysis-aba-prior-authorization-form forms, ensuring each field is accurate.