Fill out ABA forms
with AI.
ABA (Applied Behavior Analysis) forms are clinical and administrative documents used to request authorization, assessment approvals, and continued treatment coverage for ABA therapy services — most commonly for individuals diagnosed with Autism Spectrum Disorder. These forms are submitted to insurance payers, Medicaid programs, and managed care organizations to demonstrate medical necessity and secure approval before services begin or continue. Because ABA therapy often requires ongoing authorizations, providers and families may encounter these forms repeatedly throughout the course of treatment.
By continuing, you acknowledge Instafill's Privacy Policy and agree to get occasional product update and promotional emails.
About ABA forms
The people who typically need these forms include Board-Certified Behavior Analysts (BCBAs), ABA therapy agencies, and healthcare providers who must obtain prior authorization from payers such as Aetna, Blue Cross Blue Shield, Health Net, Medi-Cal, Coordinated Care, and state Medicaid programs like Alabama and New Hampshire Medicaid. Parents and caregivers may also encounter these forms when coordinating coverage for a child's therapy. Whether it's an initial assessment request, a concurrent treatment review, or a payer-specific authorization form, accurate and complete submission is critical — errors or missing information can delay or deny access to care.
These forms often require detailed clinical data, provider credentials, diagnosis codes, and service units, making them time-consuming to complete correctly. Tools like Instafill.ai use AI to fill these forms in under 30 seconds, helping providers reduce administrative burden while keeping data accurate and secure.
Forms in This Category
- Enterprise-grade security & data encryption
- 99%+ accuracy powered by AI
- 1,000+ forms from all industries
- Complete forms in under 60 seconds
How to Choose the Right Form
Selecting the correct Applied Behavior Analysis (ABA) form is critical for ensuring that clinical services are authorized without administrative delays. Most forms in this category are payer-specific, meaning your choice depends primarily on the patient’s insurance provider and the current stage of treatment.
Forms for Private Insurance Networks
If you are working with a private or commercial health plan, you must use the form specific to that carrier’s utilization management department:
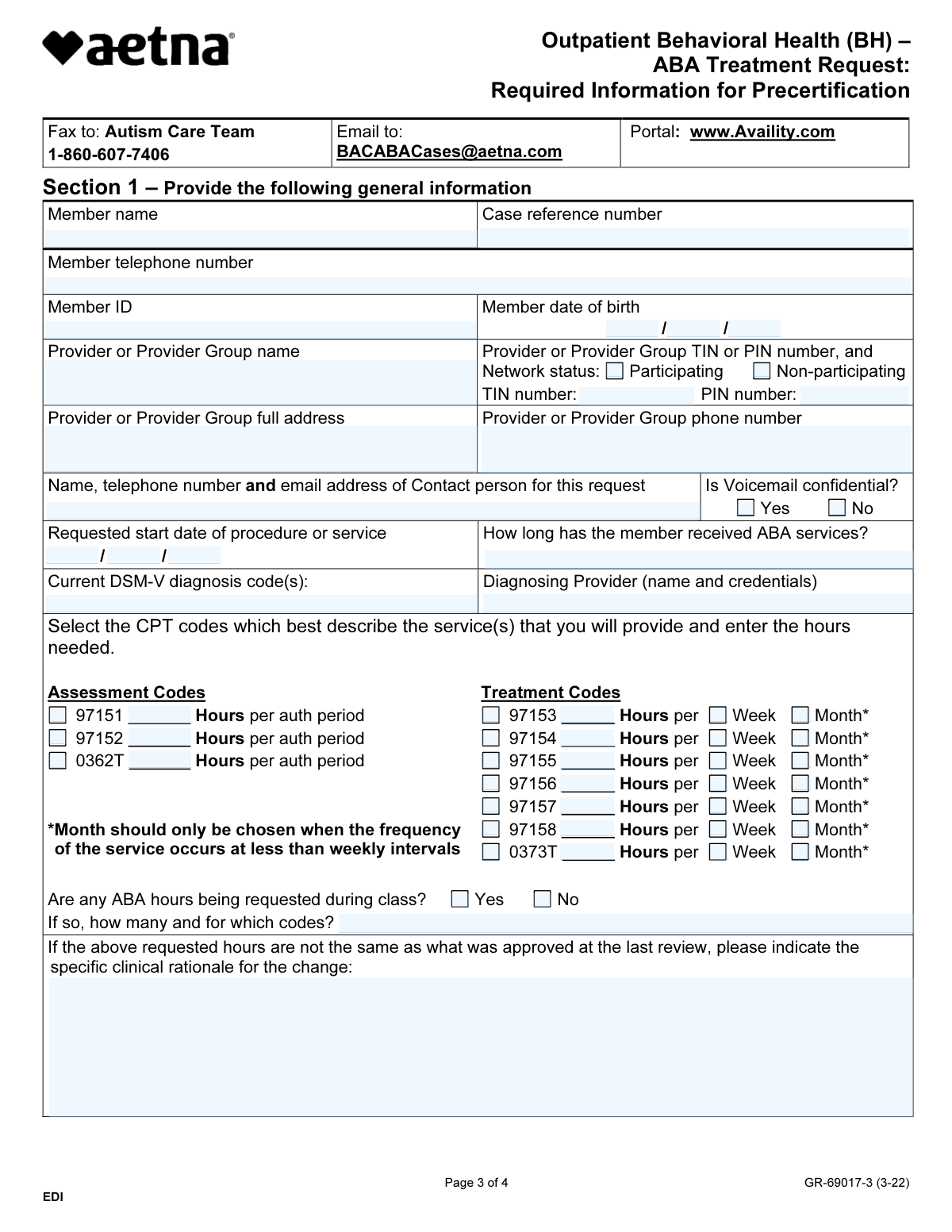
- Aetna: Use Form BHVH, Outpatient Behavioral Health – ABA Treatment Request for precertification of outpatient services.
- Health Net: Select the Applied Behavioral Analysis (ABA) Prior Authorization Request Form (Health Net Behavioral Health Autism Center) for both initial and ongoing service requests.
- Blue Cross Blue Shield of Illinois: Use the Applied Behavior Analysis (ABA) Initial Assessment Request specifically when you need approval for the diagnostic and assessment phase (CPT 97151/97152).
- MetroPlusHealth: The MetroPlusHealth Applied Behavior Analysis (ABA) Universal ABA Request Form is the standard document for member-specific diagnostic and service requests within this network.
State-Specific Medicaid Forms
For patients covered under state-funded programs, forms are strictly regulated by regional requirements:
- California (Medi-Cal): Choose the ABA Authorization Request (Medi-Cal) – Initial and Concurrent Requests. This form covers a wide range of CPT codes including social skills groups and family training.
- Alabama: Use the Alabama Medicaid Agency ABA Therapy Assessment Form specifically for CPT 97151 assessment and treatment planning.
- New Hampshire: The Applied Behavioral Analysis (ABA) Prior Authorization Form (New Hampshire) is a comprehensive document where you submit pages 1–3 for evaluations or pages 1–6 for continued treatment.
Choosing by Treatment Phase
If your provider network allows for more generalized submissions, look at the Applied Behavioral Analysis (ABA) Prior Authorization Request Form (Coordinated Care). This is an excellent choice for care coordination and recertifications, as it includes detailed sections for medications and measurable treatment goals necessary for justifying medical necessity during continued stay reviews.
Form Comparison
| Form | Primary Purpose | Payer or Plan | Scope of Services | Required Documentation |
|---|---|---|---|---|
| Form BHVH, Outpatient Behavioral Health – ABA Treatment Request | Requesting precertification for outpatient ABA therapy | Aetna and associated health plans | Outpatient behavioral health ABA treatment | Clinical details for adjudication process |
| ABA Authorization Request (Medi-Cal) – Initial and Concurrent Requests | Authorization for initial or concurrent ABA services | Medi-Cal (California Medicaid) | 1:1 therapy, assessments, and family training | Patient demographics, NPI, and treatment plan |
| MetroPlusHealth Applied Behavior Analysis (ABA) Universal ABA Request Form | Universal request for assessments or continued care | MetroPlusHealth | Initial assessment and treatment units | Diagnostic reports and treatment plan elements |
| Alabama Medicaid Agency ABA Therapy Assessment Form (6/20/19) | Clinical request for assessment and treatment planning | Alabama Medicaid Agency | CPT 97151 assessment services | DSM-5 criteria, test scores, and goals |
| Applied Behavioral Analysis (ABA) Prior Authorization Request Form (Health Net Behavioral Health Autism Center) | Utilization review for specific ABA service hours | Health Net Behavioral Health | HCPCS/CPT codes and session units | Provider TIN, NPI, and clinical rationale |
| Applied Behavior Analysis (ABA) Initial Assessment Request | Approval for initial ABA assessment period | Blue Cross Blue Shield Illinois | Assessment codes CPT 97151 and 97152 | Diagnostic practitioner details and provider attestations |
| Applied Behavioral Analysis (ABA) Prior Authorization Request Form (Coordinated Care) | Approval for starting or continuing ABA treatment | Coordinated Care | Procedure codes and care coordination | Medicaid number and ICD-10 diagnosis codes |
| Applied Behavioral Analysis (ABA) Prior Authorization Form (New Hampshire) | Authorization for evaluation or ongoing services | New Hampshire health plans | Initial evaluations and continued services | Measurable treatment goals and medication info |
Tips for ABA forms
Ensure the procedure codes, such as 97151 for assessments or 97153 for direct therapy, match the specific services being requested. Mismatched codes and unit counts are a frequent cause of authorization delays or partial denials across different payers.
Most ABA forms require supporting documents like comprehensive diagnostic evaluations or updated treatment plans to prove medical necessity. Review the 'required attachments' section carefully to ensure your submission is considered complete upon receipt and avoid a back-and-forth with the insurer.
Verify that the National Provider Identifier (NPI) and Tax ID (TIN) for both the billing agency and the rendering BCBA are correct and consistent. Inconsistent provider data can lead to administrative rejections before the clinical review process even begins.
Always specify if the form is for an initial assessment or a continuation of existing services. Concurrent requests usually require updated progress data and measurable goals, while initial requests focus more on the primary diagnostic evaluation and baseline behaviors.
AI-powered tools like Instafill.ai can complete these complex behavioral health forms in under 30 seconds with high accuracy. Your data stays secure during the process, making it a practical time-saver for providers who need to manage high volumes of authorization requests.
Many payers require information regarding school-based services or other therapy types to ensure no duplication of services. Documenting your coordination with teachers or other specialists directly on the form demonstrates a comprehensive approach to the patient's treatment plan.
Frequently Asked Questions
ABA forms are standardized documents used by healthcare providers to request authorization for Applied Behavior Analysis therapy services. They help insurance payers determine medical necessity for various treatments, including initial assessments, direct 1:1 therapy, and social skills group sessions.
These forms are generally completed by a Board-Certified Behavior Analyst (BCBA) or a clinical supervisor at a behavioral health agency. While they contain patient demographic information, the clinical data and specific service codes must be provided by the treating professional to ensure accuracy.
The correct form depends primarily on the patient’s insurance carrier and their specific health plan, such as Medi-Cal, Aetna, or Blue Cross Blue Shield. You should select the form that corresponds to the payer responsible for the patient's behavioral health benefits in their specific state.
Yes, you can fill out ABA forms using AI tools like Instafill.ai to streamline the administrative process. These tools can accurately extract data from source documents and clinical notes and place it into the required PDF fields in under 30 seconds.
When using AI-powered services, filling out complex ABA authorization forms typically takes less than 30 seconds. This technology automates the data entry process, which significantly reduces the manual workload for clinical staff and behavioral health providers.
Most initial assessment forms require patient demographics, a formal diagnosis such as Autism Spectrum Disorder, and the specific CPT codes for the evaluation period. You will also need to provide the credentials, NPI number, and Tax ID of the rendering provider or agency.
Most insurance carriers recommend submitting authorization requests at least two to three weeks before the intended start date of therapy. This lead time allows the utilization management team enough time to review the clinical documentation and issue an approval without delaying the patient's care.
An initial request is used to seek approval for the very first assessment or start of treatment for a new patient. A concurrent or continued stay request is used to renew an existing authorization and usually requires updated progress data and measurable goals to demonstrate the treatment's ongoing effectiveness.
Payers require a comprehensive diagnostic report to verify that the patient meets the clinical criteria for ABA therapy under their specific plan guidelines. This report, typically provided by a psychologist or specialized pediatrician, serves as the primary evidence for the medical necessity of the requested services.
Completed forms are typically submitted to the insurance company's utilization management or behavioral health department via a secure provider portal, fax, or mail. You should check the specific submission instructions located at the top or bottom of the form to ensure it reaches the correct department.
Glossary
- BCBA (Board Certified Behavior Analyst)
- A graduate-level professional who is certified to provide and oversee Applied Behavior Analysis services and is typically the individual responsible for completing these forms.
- CPT Codes
- Current Procedural Terminology codes, such as 97151 or 97153, used to identify specific ABA services like assessments and direct therapy for insurance billing.
- Prior Authorization
- A requirement by health plans for providers to obtain approval before delivering ABA services to ensure the treatment is covered under the patient's plan.
- Units
- The standard measurement of time used in ABA billing, where one unit usually equals 15 minutes of service provided to the patient.
- Medical Necessity
- The clinical standard used by insurers to determine if the requested ABA therapy is appropriate and essential for treating the patient's specific diagnosis.
- NPI (National Provider Identifier)
- A unique 10-digit identification number required on all HIPAA-standard healthcare transactions to identify the specific provider or agency delivering services.
- ICD-10 Code
- A standardized system of diagnostic codes used to classify the patient's condition, such as Autism Spectrum Disorder (F84.0), on authorization forms.
- Concurrent Review
- A periodic assessment by an insurance company to review a patient's progress and determine if continued ABA services are authorized after the initial period ends.