Yes! You can use AI to fill out Outpatient Behavioral Health (BH) – ABA Treatment Request: Required Information for Precertification (GR-69017-4)
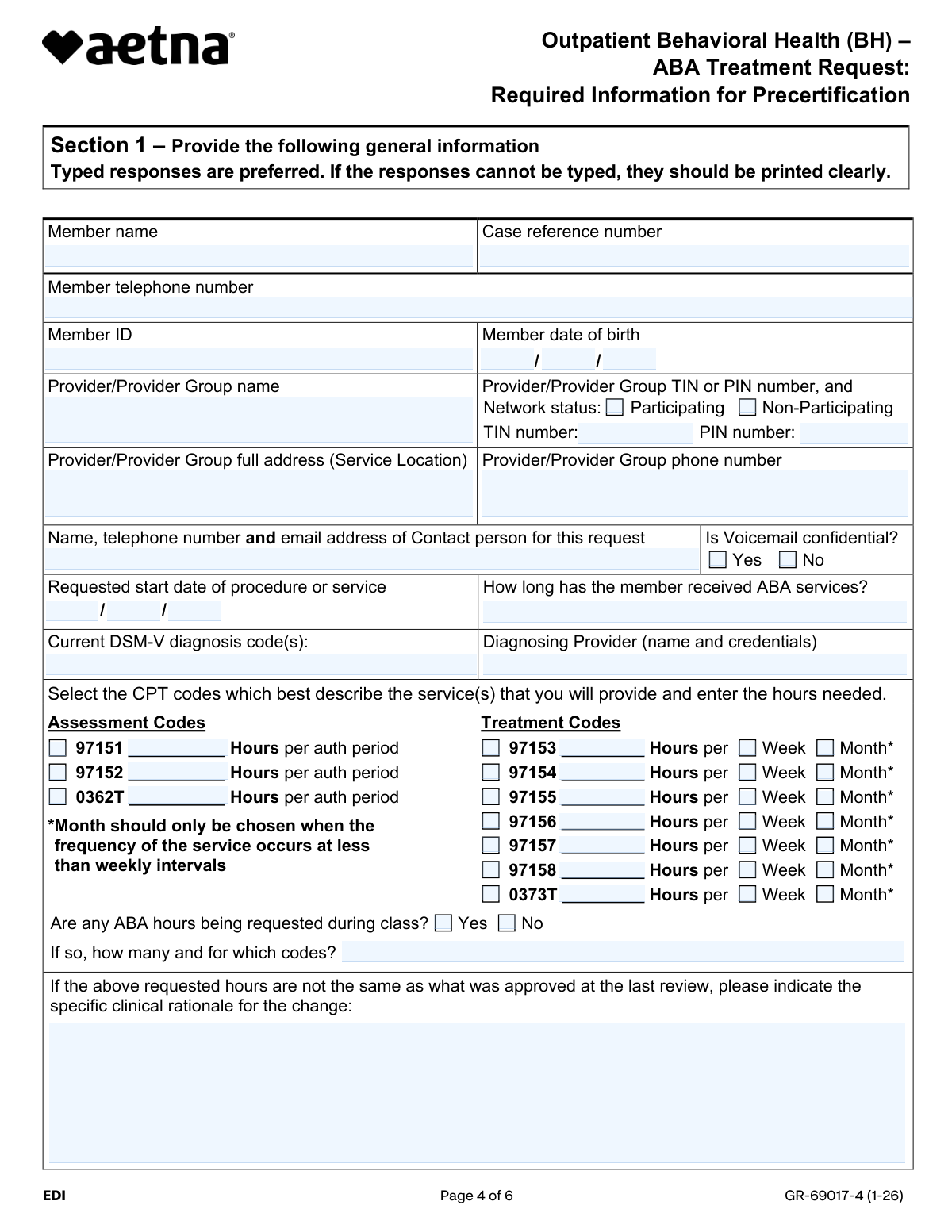
The Aetna GR-69017-4 form is an official precertification support document required by Aetna, Innovation Health, Allina Health | Aetna, and Banner | Aetna plans when requesting authorization for outpatient Applied Behavior Analysis (ABA) therapy services for members diagnosed with Autism Spectrum Disorder. Effective January 1, 2026, it replaces all prior ABA precertification information request documents and must be completed by the patient's attending provider with detailed clinical, diagnostic, and treatment information. The form captures member demographics, CPT codes, treatment hours, supervising provider credentials, essential quality care elements, and supporting documentation requirements to facilitate a medical necessity review. Today, providers can fill out this complex multi-section form quickly and accurately using AI-powered services like Instafill.ai, which can also convert non-fillable PDF versions into interactive fillable forms.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out GR-69017-4 ABA Precertification Form using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Outpatient Behavioral Health (BH) – ABA Treatment Request: Required Information for Precertification (GR-69017-4) |
| Number of pages: | 6 |
| Language: | English |
Instafill Demo: filling out a legal form in seconds
How to Fill Out GR-69017-4 ABA Precertification Form Online for Free in 2026
Are you looking to fill out a GR-69017-4 ABA PRECERTIFICATION FORM form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your GR-69017-4 ABA PRECERTIFICATION FORM form in just 37 seconds or less.
Follow these steps to fill out your GR-69017-4 ABA PRECERTIFICATION FORM form online using Instafill.ai:
- 1 Navigate to Instafill.ai and upload the GR-69017-4 ABA Precertification form or select it from the available form library to begin filling it out online.
- 2 Complete Section 1 by entering general information including the member's name, ID, date of birth, telephone number, case reference number, DSM-V diagnosis codes, diagnosing provider details, and the provider/provider group's name, address, TIN/PIN, and network status.
- 3 Select the applicable CPT assessment codes (97151, 97152, 0362T) and treatment codes (97153–97158, 0373T), entering the requested hours per week or month for each, and indicate whether any ABA hours are being requested during class.
- 4 Complete Section 2 by providing member-specific information, including the supervising ABA provider's credentials, any additional services the member is receiving, collaboration with other providers, essential elements of quality care checkboxes, and the member's areas of functional impairment.
- 5 Attach all required supporting documentation, such as standardized assessment results, the individualized treatment plan with baseline and current data, functional behavior assessment, caregiver goals, and discharge criteria.
- 6 Review Section 3 regarding the fraud acknowledgment statement to ensure all information provided is accurate and complete before signing.
- 7 Sign and complete Section 4 with the form completer's name and title, then submit the completed form electronically via Availity with the case reference number, or fax it to the Precertification Department at 860-607-7406 for commercial ABA requests.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable GR-69017-4 ABA Precertification Form Form?
Speed
Complete your GR-69017-4 ABA Precertification Form in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 GR-69017-4 ABA Precertification Form form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form GR-69017-4 ABA Precertification Form
This form is used to provide required clinical information for precertification of outpatient Applied Behavior Analysis (ABA) treatment for members with Autism Spectrum Disorder. It applies to Aetna, Innovation Health, Allina Health | Aetna, and Banner | Aetna plans. It is not used to initiate a new precertification request — that must be done separately via Availity or by phone.
The patient's attending provider must complete all sections of this form. It is intended for healthcare providers submitting clinical information to support an ABA precertification request, not for patients or caregivers to fill out themselves.
No, this form cannot be used to initiate a new precertification request. You must first submit an initial request electronically through Availity or by calling the Precertification Department, and then use this form to supply supporting clinical information if needed.
The preferred method is to submit your initial request through the Availity provider portal at Availity.com/aetnaproviders using the Authorization (Precertification) Add transaction. Alternatively, you can call the Precertification Department. Once submitted, you may be asked to complete a short questionnaire or attach this form with supporting clinical documentation.
If your request was submitted via telephone, you can either upload the form and documentation through the Availity provider portal using your reference number, or fax it to the Precertification Commercial ABA fax number: 860-607-7406. This fax line is for clinical information only.
Yes, this form should not be used for members in Maryland or Massachusetts. Providers in those states should follow the applicable state-specific precertification processes.
You should include results of a standardized assessment (e.g., Vineland, ABAS, VB-MAPP) completed within the past 12 months, a time-limited individualized treatment plan with measurable target behaviors, supporting data justifying the number of hours requested, caregiver goals, discharge criteria, and any referrals to supplemental resources. Failure to submit applicable medical records may result in a delay or denial of coverage.
The form covers assessment codes 97151, 97152, and 0362T (entered as hours per authorization period), and treatment codes 97153, 97154, 97155, 97156, 97157, 97158, and 0373T (entered as hours per week or per month). The 'per month' option should only be selected when the service frequency is less than weekly.
Section 2 requires information about who is supervising the ABA services (name, credentials, phone number), whether the member is receiving additional services such as physical therapy, speech therapy, or mental health services, confirmation of essential quality care elements, and identification of the member's areas of impairment such as self-injurious behavior, language deficits, or social/emotional challenges.
Once Aetna receives the requested documentation, a clinical review will be performed and a coverage determination will be made. You will be notified of the decision, and your administrative reference number will appear on the electronic precertification response.
Aetna uses Clinical Policy Bulletin #648: Autism Spectrum Disorders and the Applied Behavior Analysis Medical Necessity Guide to make coverage determinations. Providers are encouraged to review these resources before completing the form. They can be found on the Aetna website or via the link on the member's ID card.
If the requested hours differ from those approved at the last review, you must provide a specific clinical rationale for the change in the designated field on the form. Supporting data demonstrating the current severity level of impairment should also be attached.
Yes, AI-powered services like Instafill.ai can help you accurately auto-fill form fields, saving time and reducing errors. If the PDF version of this form is not fillable, Instafill.ai can also convert flat, non-fillable PDFs into interactive fillable forms so you can complete them digitally.
You can visit Instafill.ai, upload the ABA Treatment Request precertification form, and use the AI-powered tool to auto-fill the required fields with accurate information. This is especially helpful for lengthy forms with multiple sections, CPT codes, and clinical details, ensuring nothing is missed before submission.
For questions about how to fill out the form or the precertification process, call 1-800-424-4047 (TTY: 711). If you received a completed fax form in error, call 1-800-624-0756 (TTY: 711) or 1-888-632-3862 (TTY: 711) immediately, as the form contains confidential information.
Compliance GR-69017-4 ABA Precertification Form
Validation Checks by Instafill.ai
1
Ensures Member Date of Birth is a Valid and Logically Consistent Date
This check validates that the Member Date of Birth fields (month, day, and year) together form a real, complete calendar date in MM/DD/YYYY format. The year must reflect a plausible age for an ABA treatment recipient, and the date must not be in the future. Failure to provide a valid date of birth may result in the inability to verify member eligibility and could cause delays or denial of the precertification request.
2
Ensures Requested Start Date is a Valid Future or Near-Present Date
This check validates that the Requested Start Date of Procedure or Service fields (month, day, and year) form a valid calendar date in MM/DD/YYYY format. The requested start date should not be significantly in the past, as precertification is intended to authorize future or imminent services. If the start date is missing, invalid, or illogically far in the past, the request may be rejected or require additional clarification before processing.
3
Ensures Member Name is Fully Provided and Not Left Blank
This check confirms that the Member Name field contains a complete entry, including at minimum a first and last name, and is not left blank or filled with placeholder text. The member's full legal name is essential for accurately matching the request to the correct insurance record and member ID. An incomplete or missing name may result in the request being unprocessable or matched to the wrong member account.
4
Ensures Member ID Follows Expected Format and Is Not Blank
This check validates that the Member ID field is populated and conforms to the expected alphanumeric format used by Aetna or affiliated plan identifiers. The Member ID is the primary key used to locate the member's coverage and eligibility information in the system. A missing or incorrectly formatted Member ID will prevent the precertification team from verifying coverage and will likely result in a processing delay or denial.
5
Ensures Provider TIN or PIN Number Is Provided and Correctly Formatted
This check validates that at least one of the TIN (Taxpayer Identification Number) or PIN (Personal Identification Number) fields is populated, and that the TIN, if provided, follows the standard 9-digit format (XX-XXXXXXX). The TIN or PIN is required to identify the billing provider and verify their network participation status. If neither identifier is provided or the format is invalid, the request cannot be properly attributed to a recognized provider, which may result in denial.
6
Ensures Network Status Selection Is Mutually Exclusive (Participating or Non-Participating)
This check confirms that exactly one of the two network status options — Participating or Non-Participating — is selected, and that both are not checked simultaneously. Network status directly affects coverage determination, reimbursement rates, and whether additional authorization steps are required. If neither or both options are selected, the form is considered incomplete and the request cannot be accurately processed.
7
Ensures At Least One CPT Code Is Selected with Corresponding Hours Entered
This check validates that at least one CPT code (either an assessment code such as 97151, 97152, or 0362T, or a treatment code such as 97153–97158 or 0373T) is selected and that a corresponding number of hours is entered for each selected code. Hours must be a positive numeric value and cannot be zero or left blank when a code is checked. Without a valid CPT code and associated hours, the clinical reviewer cannot determine the scope of services being requested, which will result in an incomplete submission.
8
Ensures Treatment Code Frequency Selection Is Mutually Exclusive Per Code (Week or Month, Not Both)
For each selected treatment code (97153 through 0373T), this check confirms that exactly one frequency option — either 'Week' or 'Month' — is selected, and not both simultaneously. Additionally, the 'Month' option should only be selected when the service frequency is less than weekly, as noted in the form instructions. Selecting both or neither frequency options for a given treatment code renders the hours request ambiguous and may cause the authorization to be pended or denied.
9
Ensures 'Month' Frequency Is Only Selected When Service Occurs Less Than Weekly
This check flags any treatment code where the 'Month' frequency is selected but the corresponding hours entered suggest a weekly or more frequent service cadence. The form explicitly states that 'Month' should only be chosen when the frequency of the service occurs at less than weekly intervals. Incorrectly selecting 'Month' for frequently occurring services may misrepresent the total hours requested and lead to an inaccurate authorization or a request for additional clinical justification.
10
Ensures ABA Hours During Class Detail Is Provided When 'Yes' Is Selected
This check validates that when the 'Yes' option is selected for ABA hours being requested during class, the corresponding detail field specifying the number of hours and associated CPT codes is also completed. This information is clinically significant as it affects the setting and supervision requirements for the authorized services. If 'Yes' is selected but no detail is provided, the form is incomplete and the reviewer cannot assess the appropriateness of the in-class hours requested.
11
Ensures Clinical Rationale for Hour Change Is Provided When Hours Differ from Last Approval
This check confirms that the Clinical Rationale for Change field is populated whenever the hours requested in the current submission differ from those approved at the last review. The form explicitly requires a specific clinical explanation for any such discrepancy. Omitting this rationale when hours have changed leaves the reviewer without the necessary clinical context to justify the modification, which may result in a pended or denied authorization.
12
Ensures Supervising/Directing Provider Information Is Fully Completed
This check validates that the Supervising Director Information field in Section 2 contains all three required elements: the supervisor's full name, their credential or certification, and their phone number. The supervising provider's qualifications are a key factor in determining whether the essential element of 'Service providers are appropriately licensed/certified' is met. An incomplete entry — such as a name without credentials — may raise compliance concerns and result in the request being pended for additional information.
13
Ensures Collaboration Explanation Is Provided When 'No' Is Selected for Provider Collaboration
This check confirms that when 'No' is selected for the question about collaborating with all listed additional service providers, the explanation field ('If no, please explain why') is completed with a substantive response. Collaboration among providers is an essential element of quality ABA care, and the absence of collaboration must be clinically justified. If 'No' is selected without an explanation, the form is incomplete and the reviewer cannot assess whether the lack of collaboration is clinically appropriate.
14
Ensures At Least One Member Impairment Area Is Selected in Section 2, Question 4
This check validates that at least one impairment area checkbox is selected in the list provided in Section 2, Question 4 (e.g., self-injurious behavior, expressive/receptive language, social/emotional reciprocity). Identifying the member's specific areas of impairment is required to justify the medical necessity of ABA services and the number of hours requested. If no impairment areas are selected, the clinical reviewer lacks the foundational information needed to evaluate the appropriateness of the treatment request.
15
Ensures Current DSM-V Diagnosis Code Is Provided and Formatted Correctly
This check validates that the Current DSM-V Diagnosis Code field is populated with at least one valid ICD-10/DSM-5 diagnosis code relevant to Autism Spectrum Disorder (e.g., F84.0). The diagnosis code must follow the standard alphanumeric format and should correspond to an ASD-related condition, as ABA services are specifically indicated for this population. A missing, improperly formatted, or clinically inconsistent diagnosis code will prevent the reviewer from confirming medical necessity and may result in denial.
16
Ensures Form Completed By and Title Fields Are Populated in Section 4
This check confirms that both the 'Form completed by' and 'Title' fields in Section 4 are filled in, identifying the attending provider who is attesting to the accuracy of the information submitted. These fields serve as the provider's acknowledgment of the fraud warning stated in Section 3 and establish accountability for the clinical information provided. A form submitted without a completed signature block may be considered unsigned and therefore invalid, resulting in rejection of the precertification request.
Common Mistakes in Completing GR-69017-4 ABA Precertification Form
Many providers mistakenly submit this form as the first step in the precertification process, not realizing it is a supplemental clinical information form only. The form explicitly states it cannot be used to initiate a new precertification request — providers must first submit electronically via Availity or call the Precertification Department to obtain a reference number. Submitting this form without a prior authorization request on file will result in delays or denial of coverage. Always initiate the request through Availity or by phone first, then use this form to attach supporting clinical documentation.
Providers frequently omit the case reference number or enter an incorrect one, especially when the form is completed by administrative staff who may not have the reference number readily available. Without a valid and unique reference number, the clinical documentation cannot be matched to the correct precertification case, causing significant processing delays. The form notes that every precertification request should have a unique reference number obtained from the initial Availity submission or phone call. Always confirm and record the reference number before completing this form, and consider using tools like Instafill.ai to auto-populate validated reference numbers.
Providers sometimes select 'Month' as the frequency for treatment CPT codes (97153–0373T) out of habit or misunderstanding, when the service is actually delivered weekly. The form clearly states that 'Month' should only be chosen when the frequency of the service occurs at less than weekly intervals. Incorrectly selecting 'Month' can result in an authorization for far fewer hours than clinically needed, disrupting the member's treatment. Carefully review the frequency of each service before selecting the billing period, and double-check that monthly selections are only used for services occurring less than once per week.
A very common mistake is submitting the form without attaching all required supporting documentation, such as standardized assessment results (e.g., Vineland, ABAS, VB-MAPP) completed within the past 12 months, a time-limited individualized treatment plan with measurable goals, and data demonstrating the severity of impairment. The form explicitly states that failure to submit applicable medical records may result in a delay or denial of coverage. Providers should use the checklist in Section 2, Question 5 as a guide and ensure every applicable document is attached before submission. AI-powered tools like Instafill.ai can help flag missing documentation requirements before submission.
Providers sometimes enter an outdated, incomplete, or incorrect DSM-5 diagnosis code, such as using a non-specific code or omitting required specifiers for Autism Spectrum Disorder. An incorrect diagnosis code can trigger a clinical review denial or require additional follow-up, delaying authorization. The diagnosing provider's name and credentials must also accompany the diagnosis code, and this information is frequently left incomplete. Always verify the exact DSM-5 code with the diagnosing clinician and ensure the full code with any applicable specifiers is entered alongside the provider's full name and credentials.
Providers often confuse the Taxpayer Identification Number (TIN) with the Personal Identification Number (PIN), or leave one of these fields blank entirely. Both numbers may be required depending on the provider's setup, and entering the wrong number can cause the claim to be misrouted or rejected during the clinical review process. Additionally, failing to check the correct network status box (Participating vs. Non-Participating) is a related error that can affect reimbursement rates and authorization outcomes. Verify both numbers with your billing department before completing the form, and ensure the network status accurately reflects your current contract status with Aetna or Innovation Health.
When the number of hours requested differs from what was approved at the last review, the form requires a specific clinical rationale explaining the change, but this field is frequently left blank. Reviewers cannot approve an increase or decrease in hours without understanding the clinical basis for the change, which will result in a pended or denied request. This mistake often occurs because providers assume the supporting documentation alone is sufficient to justify the change. Always complete the clinical rationale field explicitly when hours differ from the prior authorization, referencing specific data points such as assessment results, behavioral changes, or treatment plan updates.
Providers sometimes skip or only partially complete the essential elements checklist in Section 2, Question 3, either because they assume the attached documentation covers these points or because they overlook the section entirely. Each checkbox represents a critical clinical criterion — such as primary caregiver participation and appropriately licensed service providers — that reviewers use to assess medical necessity. Leaving boxes unchecked may imply that the element is not met, even if it is, leading to unnecessary denials or requests for additional information. Review each element carefully and check all boxes that apply, ensuring the supporting documentation corroborates each checked item.
When providers check 'Yes' to indicate that ABA hours are being requested during class time, they frequently forget to specify the number of hours and the specific CPT codes associated with those in-class hours. This omission leaves reviewers without the information needed to evaluate the appropriateness of in-school ABA services, which are subject to additional scrutiny. Incomplete responses to this question can result in those hours being excluded from the authorization. If in-class ABA hours are requested, always provide both the quantity of hours and the relevant CPT codes in the space provided.
The form explicitly states it should not be used for members in Maryland or Massachusetts, yet providers occasionally submit it for members in these states, particularly when managing large caseloads across multiple states. Using this form for excluded states can result in the request being rejected outright or processed under incorrect guidelines, causing significant delays. Providers should verify the member's state of residence before completing the form and use the appropriate state-specific forms or processes for Maryland and Massachusetts. Maintaining a clear internal checklist or using automated form-routing tools can help prevent this error.
Providers often enter only a name for the contact person without including the telephone number and email address, or they forget to indicate whether the voicemail is confidential. Incomplete contact information means that Aetna's clinical reviewers cannot reach the appropriate person if they have questions, which can delay the authorization decision. The voicemail confidentiality question is particularly important for HIPAA compliance, as it determines whether protected health information can be left in a voicemail message. Always provide the full name, direct phone number, and email address of the contact person, and clearly indicate the voicemail confidentiality status.
In Section 2, Question 2, when providers indicate they do not collaborate with all listed supplemental service providers (e.g., speech therapists, school services, prescribing physicians), they frequently leave the explanation field blank. Reviewers require a clear explanation of why collaboration is not occurring, as coordination of care is a key component of ABA medical necessity criteria. Without this explanation, the lack of collaboration may be interpreted as a gap in care quality, potentially resulting in a denial. If collaboration is not occurring with any listed provider, provide a specific and clinically sound explanation, such as the member not currently receiving that service or a documented referral being in progress.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out GR-69017-4 ABA Precertification Form with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills outpatient-behavioral-health-bh-aba-treatment-request-required-information-for-precertification-gr-69017-4 forms, ensuring each field is accurate.