Yes! You can use AI to fill out Arkansas Medicaid Applied Behavioral Analysis (ABA) Authorization Request
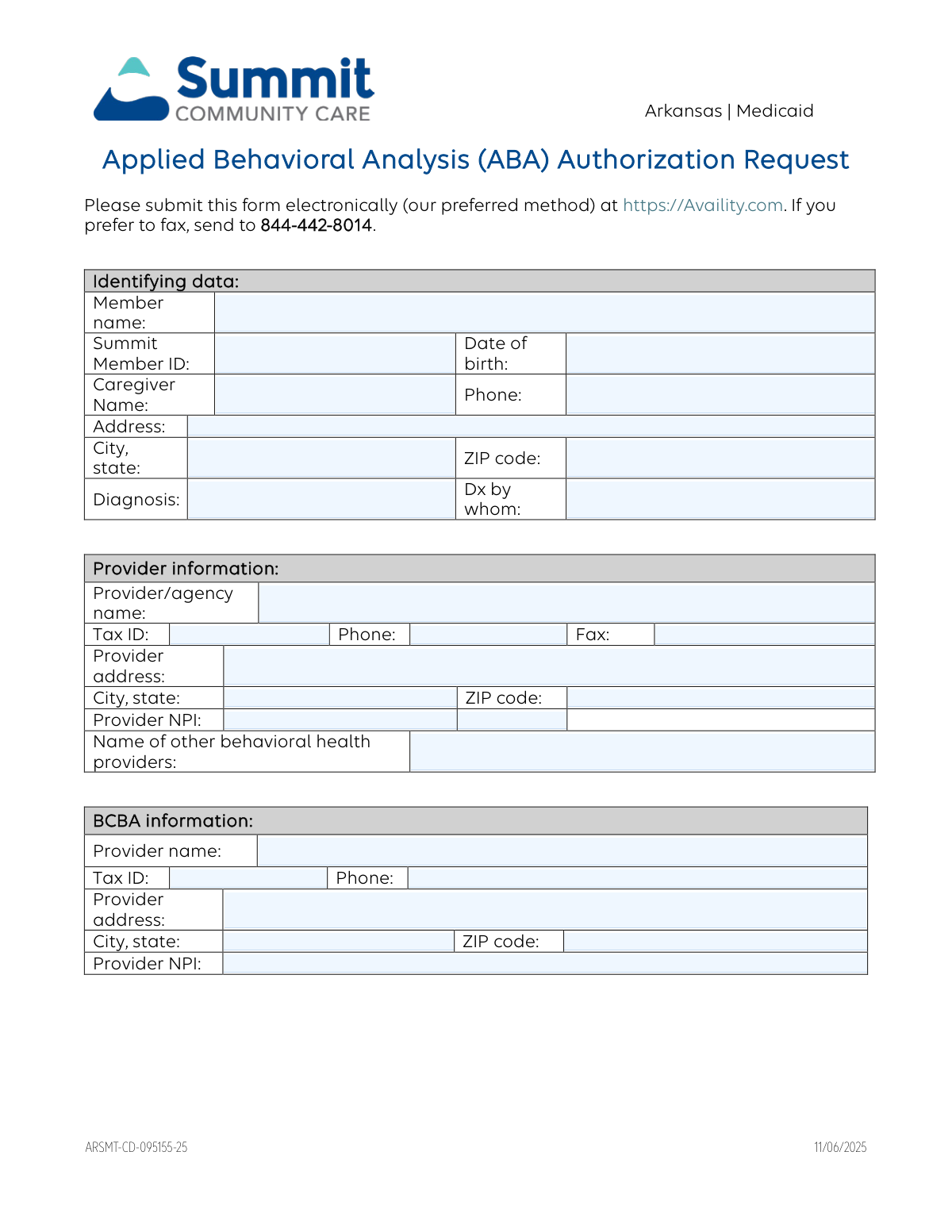
The Arkansas Medicaid Applied Behavioral Analysis (ABA) Authorization Request (ARSMT-CD-095155-25) is an official form used by behavioral health providers and BCBAs to request prior authorization from Summit Community Care for ABA therapy services for Medicaid-enrolled members. The form captures member identifying information, provider and BCBA details, PCP information, DSM-V diagnoses, current medications, treatment goals, behavior reduction plans, functional assessment results, and specific service authorization codes (97151, 97153, 97155, 97156) with requested hours and units. It is a critical document ensuring that ABA services are medically necessary, clinically justified, and properly coordinated before services are rendered. Today, this form can be filled out quickly and accurately using AI-powered services like Instafill.ai, which can also convert non-fillable PDF versions into interactive fillable forms.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out ARSMT-CD-095155-25 using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Arkansas Medicaid Applied Behavioral Analysis (ABA) Authorization Request |
| Number of pages: | 6 |
| Language: | English |
Instafill Demo: filling out a legal form in seconds
How to Fill Out ARSMT-CD-095155-25 Online for Free in 2026
Are you looking to fill out a ARSMT-CD-095155-25 form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your ARSMT-CD-095155-25 form in just 37 seconds or less.
Follow these steps to fill out your ARSMT-CD-095155-25 form online using Instafill.ai:
- 1 Navigate to Instafill.ai and upload the Arkansas Medicaid ABA Authorization Request form (ARSMT-CD-095155-25) or select it from the available form library.
- 2 Enter the member's identifying information, including full name, Summit Member ID, date of birth, caregiver name and phone number, and member address.
- 3 Complete the provider and BCBA information sections, including agency name, Tax ID, NPI, phone, fax, and address for both the treating provider and the Board Certified Behavior Analyst (BCBA).
- 4 Fill in the PCP information, DSM-V diagnoses, and current medications with dosages and frequencies, and indicate whether the provider is participating or non-participating in Summit Community Care's network.
- 5 Provide the clinical assessment and treatment details, including baseline behaviors, treatment goals, behavior reduction plan, functional assessment results, behavior improvement plan, parent/guardian training goals, and justification for the requested ABA therapy hours.
- 6 Complete the requested service authorization table by entering the applicable CPT codes (97151, 97153, 97155, 97156) with modifier codes, start and end dates, hours and units requested per week, and total units requested.
- 7 Review the treatment plan coordination section, check the appropriate boxes for permission to release information and treatment plan agreement, provide any required rationale, enter the signature date, and electronically sign before submitting the form via Availity.com or faxing to 844-442-8014.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable ARSMT-CD-095155-25 Form?
Speed
Complete your ARSMT-CD-095155-25 in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 ARSMT-CD-095155-25 form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form ARSMT-CD-095155-25
This form is used to request prior authorization for Applied Behavioral Analysis (ABA) therapy services through Summit Community Care under Arkansas Medicaid. It covers both the initial functional assessment and the ongoing ABA-based therapy services for members diagnosed with Autism Spectrum Disorder.
This form must be completed by a licensed care provider or agency (such as a BCBA or qualified healthcare professional) who is requesting ABA therapy services on behalf of an Arkansas Medicaid member. Both the treating provider/agency and the Board Certified Behavior Analyst (BCBA) information must be included.
The preferred method is to submit the form electronically through Availity at https://Availity.com. If you prefer to fax, you can send the completed form to 844-442-8014. Electronic submission is recommended for faster processing.
The authorization process involves two steps: first, a prior authorization (PA) is requested to approve the functional assessment and development of a behavior treatment plan; second, a separate PA is required to approve the actual provision of ABA-based therapy services. Both steps must be completed before services can begin.
Care providers may request a review for up to 180 days, which equals a six-month authorization period. The request must specify whether services are based on a focused or comprehensive service delivery model.
For initial assessment requests, you must attach interdisciplinary reports confirming the Autism diagnosis, prescription and referral forms if available, and a treatment plan dated within 30 days of the start date. The submission should also include a current behavioral support plan, functional assessment results, parent involvement documentation, and a discharge/transition plan.
This form supports authorization requests for four CPT codes: 97151 (Behavior identification assessment), 97153 (Adaptive behavior treatment by protocol administered by a technician), 97155 (Adaptive behavior treatment with protocol modification by a qualified professional), and 97156 (Family adaptive behavior treatment guidance). Each code is billed in 15-minute units.
If you are a non-participating provider, you must indicate this on the form and confirm whether you accept Summit Community Care's out-of-network fee schedule. If you do not accept the fee schedule, Summit Community Care retains the right to redirect the member to a participating provider if the requested services are available within their network.
The treatment plan must include a current behavioral support plan, symptoms and behaviors requiring treatment, skills to be addressed, baseline measures, current progress, desired outcomes in measurable terms, a list of other services the member receives, the treatment schedule (hours per day/week), documentation of parental involvement with measurable goals, and measurable discharge criteria and a transition plan.
Yes, the provider must indicate whether they have requested permission from the patient's parent or guardian to release information to the Primary Care Provider (PCP), and whether the treatment plan was discussed with and agreed upon by the patient's parent or guardian. If either answer is 'No,' a written rationale must be provided.
No, requests for psychological or neuropsychological testing require a separate form. This ABA Authorization Request form is specifically for ABA therapy services and related assessments only.
Yes, the provider must indicate the predominant location where services will take place by selecting Home, Clinic, School, or Other (with a written specification). This information is required as part of the authorization request.
Yes, AI-powered services like Instafill.ai can help you accurately auto-fill the fields on this form, saving time and reducing errors. If you have a flat, non-fillable PDF version of this form, Instafill.ai can also convert it into an interactive fillable form so you can complete it digitally.
To fill out this form online, visit Instafill.ai and upload the ABA Authorization Request PDF. The AI will guide you through each field—member information, provider details, BCBA information, treatment plan, and service codes—auto-filling where possible and flagging any missing required information before you submit.
The justification section requires the provider to supply specific clinical information explaining why the number of ABA therapy hours requested is medically necessary for the member. This is a critical part of the authorization review, as Summit Community Care uses this information to determine whether the requested hours are appropriate based on the member's needs and treatment goals.
Compliance ARSMT-CD-095155-25
Validation Checks by Instafill.ai
1
Ensures Member Date of Birth is a Valid Date in the Past
This check verifies that the Member Date of Birth field contains a properly formatted date (MM/DD/YYYY) and that the date falls in the past, not in the future. Since this is an ABA authorization request typically for pediatric members with Autism diagnoses, the date should also reflect a plausible age range for ABA therapy recipients. If this validation fails, the form cannot be processed as the member's identity and eligibility cannot be confirmed.
2
Ensures Provider and BCBA NPI Numbers are Valid 10-Digit Identifiers
This check validates that all National Provider Identifier (NPI) fields — for the Provider/Agency, BCBA, and PCP — contain exactly 10 numeric digits, conforming to the CMS NPI format standard. NPI numbers are critical for billing and credentialing verification within the Medicaid system, and an invalid NPI will result in claim rejection or inability to verify provider participation. If any NPI field contains non-numeric characters, fewer or more than 10 digits, or is left blank, the submission should be flagged for correction.
3
Ensures Tax ID Fields are Properly Formatted for Provider, BCBA, and PCP
This check verifies that all Tax Identification Number (Tax ID) fields for the Provider/Agency, BCBA provider, and PCP are formatted as a valid 9-digit Employer Identification Number (EIN) in the format XX-XXXXXXX. Tax IDs are required for Medicaid reimbursement processing and provider verification, and an incorrectly formatted or missing Tax ID will prevent payment and authorization processing. The validation should reject entries that contain letters, special characters other than a hyphen, or an incorrect digit count.
4
Ensures Authorization Date Range Does Not Exceed 180-Day Maximum
This check confirms that the difference between the Start Date and End Date for each requested service code (97151, 97153, 97155, 97156) does not exceed 180 days, as specified in the form's authorization policy. The form explicitly states that care providers may request a review for up to 180 days, which equals a six-month authorization period. If any service row's date range exceeds this limit, the request must be flagged, as it falls outside the allowable authorization window and will be denied.
5
Ensures Service Authorization Start Date is Not in the Past
This check validates that the Start Date entered for each requested service code is not a date that has already passed at the time of submission, ensuring the authorization request is prospective and actionable. Submitting a prior authorization with a start date in the past may indicate a retroactive request, which typically requires separate handling under Medicaid guidelines. If a start date is found to be in the past, the submission should be flagged with a warning prompting the submitter to confirm or correct the date.
6
Ensures Total Units Requested is Mathematically Consistent with Weekly Units and Date Range
This check verifies that the Total Units Requested field for each service code is consistent with the Units Requested Per Week multiplied by the number of weeks in the authorization period defined by the Start and End Dates. Inconsistencies between these values suggest data entry errors that could result in over- or under-authorization of services, leading to billing discrepancies or member care gaps. If the calculated total does not match the entered total, the form should be flagged and the submitter prompted to reconcile the values.
7
Ensures Treatment Plan Date is Within 30 Days of the Requested Service Start Date
This check validates that the Treatment Plan referenced in the assessment and treatment section is dated within 30 days of the start date entered in the service authorization table, as explicitly required by the form instructions. An outdated treatment plan may indicate that the clinical information is no longer current, which could result in denial of the authorization request. If the treatment plan date falls outside this 30-day window, the submission should be flagged with a message directing the provider to update the treatment plan before resubmitting.
8
Ensures Non-Participating Provider and Fee Schedule Acceptance Checkboxes are Logically Consistent
This check verifies that if the 'Non-participating Provider: Yes' checkbox is selected, the submitter has also made a selection for the 'Fee Schedule Acceptance' question (Yes or No), since this question is only relevant for non-participating providers. Additionally, if 'Non-participating Provider: No' is selected, the fee schedule acceptance question should either be left blank or flagged as not applicable to avoid confusion. Failure to complete this logical pairing may result in processing delays or misrouting of the authorization request.
9
Ensures Permission Request and Treatment Plan Discussion Checkboxes Have Rationale When 'No' is Selected
This check confirms that if either the 'Permission Request: No' or 'Treatment Plan Discussion: No' checkbox is selected, the corresponding rationale text field is populated with a non-empty explanation. These fields are required by the form when consent or discussion did not occur, as they provide the clinical or legal justification necessary for Medicaid compliance. If a 'No' box is checked but the rationale field is left blank, the submission should be blocked until a rationale is provided.
10
Ensures All Phone and Fax Number Fields Contain Valid 10-Digit US Phone Numbers
This check validates that all phone and fax number fields — including Caregiver Phone, Provider Phone, Provider Fax, BCBA Phone, PCP Phone, and PCP Fax — contain a valid 10-digit US telephone number, formatted as (XXX) XXX-XXXX or XXX-XXX-XXXX. Invalid or incomplete phone numbers will prevent Summit Community Care from contacting providers or caregivers for follow-up, potentially delaying or denying the authorization. Entries containing letters, fewer than 10 digits, or invalid area codes should be flagged for correction.
11
Ensures ZIP Code Fields Contain Valid 5-Digit or ZIP+4 Format
This check verifies that all ZIP code fields — for the member, provider, BCBA provider, and PCP — contain either a valid 5-digit ZIP code or a ZIP+4 code in the format XXXXX-XXXX. Accurate ZIP codes are necessary for geographic eligibility verification, provider network determination, and correspondence routing within the Arkansas Medicaid system. ZIP code fields containing letters, special characters, or fewer than 5 digits should be flagged as invalid.
12
Ensures DSM-V Diagnosis is Consistent with ABA Therapy Eligibility Requirements
This check verifies that the DSM-V Diagnosis field contains a diagnosis code or description consistent with Autism Spectrum Disorder (ASD), as ABA therapy authorization under Arkansas Medicaid is specifically indicated for ASD diagnoses. The diagnosis entered in the DSM-V field should also be consistent with the diagnosis listed in the Diagnosis field in the member identification section. If the diagnoses are inconsistent or the DSM-V diagnosis does not reflect an ASD-related condition, the submission should be flagged for clinical review before processing.
13
Ensures Provider Signature and Signature Date are Both Present
This check confirms that both the Provider Signature field and the Signature Date field are completed before the form is submitted, as an unsigned or undated authorization request is not legally valid for Medicaid processing. The Signature Date should also be a valid calendar date that is on or before the submission date, ensuring the provider attested to the information at the time of or prior to submission. If either field is missing, the form should be blocked from submission with a clear error message directing the provider to complete the signature section.
14
Ensures at Least One Predominant Service Location Checkbox is Selected
This check verifies that at least one of the service location checkboxes — Home, Clinic, School, or Other — is selected in the 'Predominant location where services will take place' section. The service location is a required clinical detail that informs the authorization decision and care coordination planning. If no location is selected, or if 'Other' is selected but the specification field is left blank, the submission should be flagged as incomplete and the provider prompted to provide this information.
15
Ensures Medication Entries Include Dosage and Frequency When a Medication Name is Provided
This check validates that for each medication row where a medication name has been entered, the corresponding Dosage and Frequency fields are also populated. Incomplete medication information can create clinical safety risks and may result in the authorization reviewer lacking sufficient information to assess potential behavioral impacts of current medications. Any medication row with a name but missing dosage or frequency should be flagged, and the provider should be prompted to complete all three fields for each medication listed.
16
Ensures Behavior Reduction Plan Includes Baseline Frequency, Duration, Latency, and Intensity
This check verifies that the Behavior Reduction Plan field contains substantive content addressing all four required behavioral dimensions: baseline frequency, duration, latency, and intensity of problem behaviors, as explicitly required by the form instructions. These four components are essential for clinical reviewers to assess the severity of the member's behaviors and the appropriateness of the requested ABA therapy hours. If the field is blank or contains only generic text without reference to these specific dimensions, the submission should be flagged for clinical documentation deficiency.
Common Mistakes in Completing ARSMT-CD-095155-25
Providers often confuse the Summit Community Care Member ID with the Medicaid ID or other insurance identifiers, or they transpose digits when entering the number manually. An incorrect Member ID will cause the authorization request to be rejected or matched to the wrong member, delaying care. Always verify the Summit Member ID directly from the member's Summit Community Care insurance card or eligibility verification through Availity before submitting. AI-powered tools like Instafill.ai can help validate member ID formats to reduce transcription errors.
The form requires separate NPI numbers for the provider/agency and the BCBA, and submitters frequently enter the same NPI for both or leave the BCBA NPI blank. NPIs are 10-digit numbers and must correspond to the specific individual or organization rendering services; using the wrong NPI can result in claim denial or authorization mismatch. Verify each NPI through the NPPES registry (npiregistry.cms.hhs.gov) before completing the form. Tools like Instafill.ai can auto-populate and validate NPI numbers to prevent this error.
For initial assessment requests, the form explicitly requires interdisciplinary reports confirming the Autism diagnosis, yet providers frequently submit the form without these attachments, assuming the diagnosis information entered on the form is sufficient. Missing documentation is one of the most common reasons for authorization denials and delays in ABA services. Ensure all supporting documents—including the autism diagnosis report, prescription, and referral forms—are compiled and attached before submission. Create a checklist of required attachments to review before every submission.
The form clearly states that the Treatment Plan must be dated within 30 days of the start date, but providers often submit outdated treatment plans, especially when reusing documentation from previous authorization periods. This results in automatic denial of the request and requires resubmission with an updated plan. Always check the date on the treatment plan against the requested start date before submitting, and update the plan if it falls outside the 30-day window.
Each ABA service code (97151, 97153, 97155, 97156) is billed in 15-minute increments, meaning one hour equals four units. Providers frequently enter hours instead of units, or miscalculate total units by not multiplying weekly units by the number of weeks in the authorization period (up to 26 weeks for a 180-day period). Incorrect unit calculations lead to authorization for the wrong amount of service, causing billing issues later. Double-check all unit conversions and totals before submitting, and consider using Instafill.ai to automate these calculations.
The form requires specific, behavioral, and measurable terms for treatment goals, behavior reduction plans, and discharge criteria, but providers often submit generic or narrative descriptions that do not include baseline frequency, duration, latency, and intensity of problem behaviors. Vague clinical information is a leading cause of authorization denials, as reviewers cannot assess medical necessity without quantifiable data. Use standardized measurement tools and ensure every goal includes a baseline measure, target behavior, and measurable outcome criterion.
The 'Justification for ABA Therapy Hours Requested' field requires specific clinical information explaining why the number of hours requested is medically necessary, yet providers often leave this field blank or write only a brief sentence. Insufficient justification is a primary driver of authorization denials and peer-to-peer review requests. Clearly document the clinical rationale, referencing assessment results, severity of behaviors, and the member's functional level to support the specific number of hours requested.
The form instructions state that the care provider must specify whether services are based on a focused or comprehensive service delivery model, but many providers overlook this requirement entirely. Omitting this distinction can result in the request being returned as incomplete or reviewed under the wrong criteria. Clearly document the chosen model within the clinical narrative or treatment plan sections, and ensure it aligns with the number of hours and service codes being requested.
Providers frequently skip the three yes/no questions on page 2 regarding non-participating provider status, previous member contact, and acceptance of the out-of-network fee schedule. Leaving these unchecked creates ambiguity and may result in the request being returned or the member being redirected to a participating provider without the submitter's knowledge. Review and answer all three checkbox questions carefully, understanding that declining the out-of-network fee schedule may result in the member being redirected to another provider.
The form requires separate Tax ID numbers for the provider/agency and the BCBA provider, and submitters often enter the same Tax ID for both or use an individual SSN instead of the organization's EIN. A mismatched or incorrect Tax ID will cause payment and credentialing issues even if the authorization is approved. Verify each Tax ID against credentialing records and ensure the correct entity's Tax ID is used for each respective section.
Providers frequently leave the discharge/transition plan and parent/guardian training and support goals sections blank, treating them as optional when they are required components of a complete ABA authorization request. Missing these sections signals to reviewers that the treatment plan lacks a clear endpoint and family involvement, which can result in denial or a request for additional information. Document specific, measurable discharge criteria and concrete parent training goals that align with the overall treatment plan.
The final section of the form requires providers to confirm whether the treatment plan was discussed with the patient/guardian and whether permission was obtained to release information to the PCP, but these checkboxes are often left blank or the 'No' box is checked without providing the required rationale. Incomplete consent documentation can delay processing and raise compliance concerns. Always complete both checkboxes and, if 'No' is selected for either, provide a clear written rationale in the corresponding field before signing and dating the form.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out ARSMT-CD-095155-25 with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills arkansas-medicaid-applied-behavioral-analysis-aba-authorization-request forms, ensuring each field is accurate.