Yes! You can use AI to fill out Applied Behavior Analysis (ABA) Initial Assessment Request and Clinical Service Request Form – Blue Cross and Blue Shield of Illinois (BCBSIL)
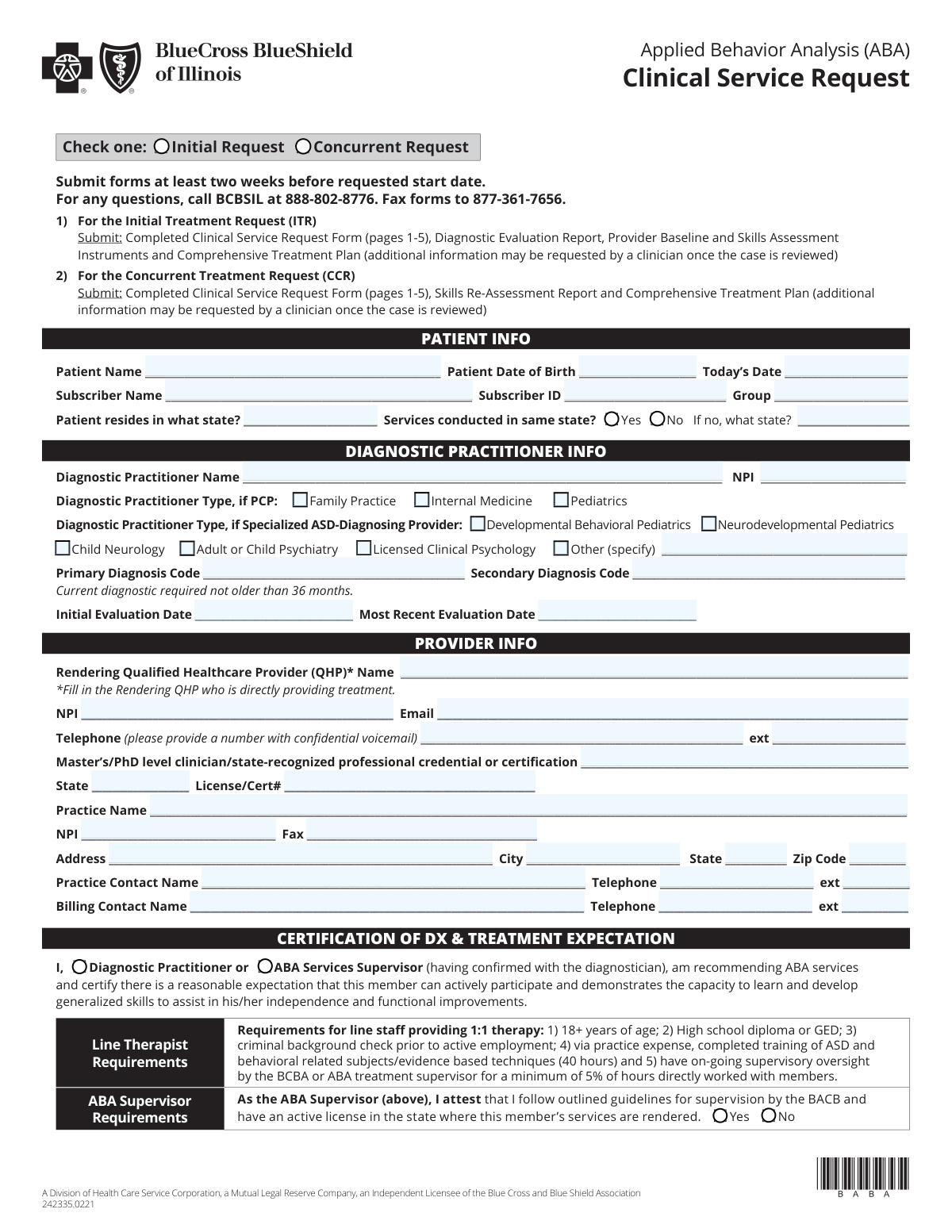
The BCBSIL Applied Behavior Analysis (ABA) Initial Assessment and Clinical Service Request form is a comprehensive authorization document submitted by qualified healthcare providers to obtain approval for ABA therapy services—including assessments, direct treatment, family training, and group treatment—for members with an ASD diagnosis covered under a BCBSIL health plan. The form captures patient demographics, diagnostic practitioner details, provider credentials, treatment history, behavioral assessments, treatment plans, parent involvement goals, fade/discharge plans, and weekly therapy schedules. Accurate and complete submission is critical to ensure timely authorization and uninterrupted care for the member. Today, providers can fill out this complex multi-page form quickly and accurately using AI-powered services like Instafill.ai, which can also convert non-fillable PDF versions into interactive fillable forms.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out BCBSIL ABA Initial Assessment & Clinical Service Request using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Applied Behavior Analysis (ABA) Initial Assessment Request and Clinical Service Request Form – Blue Cross and Blue Shield of Illinois (BCBSIL) |
| Number of pages: | 5 |
| Language: | English |
Instafill Demo: filling out a legal form in seconds
How to Fill Out BCBSIL ABA Initial Assessment & Clinical Service Request Online for Free in 2026
Are you looking to fill out a BCBSIL ABA INITIAL ASSESSMENT & CLINICAL SERVICE REQUEST form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your BCBSIL ABA INITIAL ASSESSMENT & CLINICAL SERVICE REQUEST form in just 37 seconds or less.
Follow these steps to fill out your BCBSIL ABA INITIAL ASSESSMENT & CLINICAL SERVICE REQUEST form online using Instafill.ai:
- 1 Navigate to Instafill.ai and upload the BCBSIL ABA Initial Assessment and Clinical Service Request PDF, or search for it in the Instafill.ai form library to open an interactive fillable version.
- 2 Complete the Patient Information section by entering the patient's full name, date of birth, subscriber name, subscriber ID, group number, state of residence, and state where services will be conducted.
- 3 Fill in the Diagnostic Practitioner Information section, including the practitioner's name, NPI, contact details, practitioner type (PCP or specialized ASD-diagnosing provider), primary and secondary diagnosis codes, and initial and most recent evaluation dates.
- 4 Enter the Rendering Provider and Practice Information, including the QHP's name, NPI, email, telephone, credentials, practice name, address, and billing and contact details, then complete the Certification of DX & Treatment Expectation section.
- 5 Complete the Provider Treatment Request section by specifying the request start date, service intensity (Focused or Comprehensive), total requested hours per week, and the number of 15-minute units for each applicable ABA procedure code (97151–97158).
- 6 Fill out the clinical sections including ABA Treatment History, Medical History (medications, sleep and eating issues), Baseline & Assessment Info, Current Maladaptive Behaviors, Member Treatment Plan goals, Parent Involvement training goals, and the Treatment Fade/Transition/Discharge Plan.
- 7 Enter the Member ABA Schedule and School/Other Therapy Schedule for each day of the week, indicate supports outside ABA treatment (school program type, IEP/ISP status, other therapies, coordination of care), then review all entries and submit the completed form to BCBSIL by faxing to 877-361-7656 or via the appropriate submission method.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable BCBSIL ABA Initial Assessment & Clinical Service Request Form?
Speed
Complete your BCBSIL ABA Initial Assessment & Clinical Service Request in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 BCBSIL ABA Initial Assessment & Clinical Service Request form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form BCBSIL ABA Initial Assessment & Clinical Service Request
These forms are used to request authorization for Applied Behavior Analysis (ABA) services through Blue Cross and Blue Shield of Illinois (BCBSIL). There are two main forms: the Initial Assessment Request (to authorize an ABA evaluation) and the Clinical Service Request (to authorize ongoing ABA treatment, either as an Initial Treatment Request or a Concurrent/renewal request).
These forms are completed by ABA providers, including the Board Certified Behavior Analyst (BCBA) or ABA Supervisor and the Rendering Qualified Healthcare Provider (QHP) who is directly providing treatment. The diagnosing practitioner's information is also required. Parents or caregivers do not submit these forms themselves — the provider's office handles submission.
Completed forms should be faxed to BCBSIL at 877-361-7656. For any questions during the process, you can call BCBSIL at 888-802-8776. The Clinical Service Request form must be received within 30 days of the treatment request start date.
BCBSIL requires the Clinical Service Request form to be submitted at least two weeks before the requested start date. If the form is not received within 30 days of the treatment request start date, claims should be submitted through the normal process and you will receive further instructions.
For an Initial Treatment Request, you must submit the completed Clinical Service Request Form (all 5 pages), a Diagnostic Evaluation Report, Provider Baseline and Skills Assessment Instruments, and a Comprehensive Treatment Plan. Additional information may be requested by a clinician once the case is reviewed.
For a Concurrent Treatment Request (renewal), you must submit the completed Clinical Service Request Form (all 5 pages), a Skills Re-Assessment Report, and a Comprehensive Treatment Plan. Additional information may be requested by a clinician after the case is reviewed.
The current diagnosis must not be older than 36 months. Additionally, the baseline assessment completed by the ABA provider must be within the last 30 days of the request submission date.
The form uses standard ABA CPT codes including 97151 (Assessment), 97152 (Assessment with Tech), 97153 (Direct Treatment), 97154 (Group Treatment, Tech), 97155 (Protocol Modification & Supervision), 97156 (Family Treatment), 97157 (Multi-Family Treatment), and 97158 (Group Treatment, QHP). Each unit equals 15 minutes of service, so you must enter the total number of 15-minute units requested for the assessment or treatment period.
Line therapists must: (1) be 18 years of age or older; (2) have a high school diploma or GED; (3) pass a criminal background check prior to employment; (4) complete 40 hours of training in ASD and behavioral/evidence-based techniques at the practice's expense; and (5) receive ongoing supervisory oversight by a BCBA or ABA treatment supervisor for a minimum of 5% of hours directly worked with members.
The ABA Supervisor must attest that they follow the BACB's outlined guidelines for supervision and hold an active license in the state where the member's services are rendered. By signing the form, the supervisor also certifies that all line therapists meet the required qualifications and that any staff changes will require new staff to meet the same standards.
BCBSIL requires providers to select one recognized standardized instrument to be used throughout the member's entire treatment episode so progress can be consistently measured. Accepted instruments include the VB-MAPP, ABLLS, AFLS, ABAS, and the Vineland. Standardized measurement scoring summaries should be attached if the member has been in prior treatment.
Yes, the form requires a Treatment Fade/Transition/Discharge Plan, which must include measurable fade plan criteria, a discharge plan with objective and measurable criteria, other referrals or supports recommended at discharge, and confirmation of whether the parent or caregiver is in agreement with the plan.
Yes — services like Instafill.ai use AI to accurately auto-fill form fields, saving providers significant time when completing complex multi-page forms like these BCBSIL ABA requests. If you have a flat, non-fillable PDF version of the form, Instafill.ai can also convert it into an interactive fillable form so you can complete it digitally.
To fill out these forms online, visit Instafill.ai and upload the BCBSIL ABA form PDF. The AI will guide you through each field — including patient info, provider details, diagnosis codes, procedure code units, and schedules — and auto-fill information where possible. Once complete, you can download the filled form and fax it to BCBSIL at 877-361-7656.
Both the Initial Assessment Request and the Clinical Service Request ask whether services are conducted in the same state as the patient's residence. If services are provided in a different state, you must indicate which state the services are conducted in, as this may affect coverage and authorization requirements.
Compliance BCBSIL ABA Initial Assessment & Clinical Service Request
Validation Checks by Instafill.ai
1
Ensures Patient Date of Birth is a Valid Date in the Past
This check verifies that the Patient Date of Birth field contains a properly formatted date (MM/DD/YYYY) and that the date falls in the past, not in the future or today's date. It also confirms the patient's age is plausible for ABA services (typically under 21, though adult services exist). If this validation fails, the form cannot be processed as the patient's identity and eligibility cannot be confirmed, and age-appropriate treatment planning cannot occur.
2
Ensures NPI Numbers Are 10-Digit Numeric Values
This check validates that all National Provider Identifier (NPI) fields — including those for the Diagnostic Practitioner, Facility, BCBA, Rendering QHP, and Practice — contain exactly 10 numeric digits with no letters or special characters, conforming to the CMS NPI standard. NPIs are required for billing and provider identification with BCBSIL, and an invalid NPI will result in claim rejection or authorization denial. If any NPI field fails this check, the submission must be returned for correction before processing can begin.
3
Ensures Exactly One Diagnostic Practitioner Type Is Selected
This check confirms that one and only one practitioner type checkbox is selected — either a PCP type (Family Practice, Internal Medicine, or Pediatrics) or a Specialized ASD-Diagnosing Provider type (Developmental Behavioral Pediatrics, Neurodevelopmental Pediatrics, Child Neurology, Adult or Child Psychiatry, Licensed Clinical Psychology, or Other). Selecting both a PCP type and a Specialized type, or selecting none, creates ambiguity about the practitioner's qualifications and role in the diagnosis. If 'Other' is selected, the specification field must also be populated.
4
Ensures Primary Diagnosis Code Is Present and ASD-Related
This check verifies that the Primary Diagnosis Code field is not blank and contains a valid ICD-10 code, and flags if the code does not fall within the expected Autism Spectrum Disorder range (e.g., F84.0, F84.5) or other qualifying diagnoses for ABA services. ABA services through BCBSIL require a qualifying ASD diagnosis, and an absent or non-qualifying diagnosis code will result in automatic denial of the authorization request. If the primary diagnosis code is missing or invalid, the form must be returned to the submitting provider.
5
Ensures Diagnostic Evaluation Date Is Not Older Than 36 Months
This check validates that the Most Recent Evaluation Date is within 36 months of the Request Submission Date or Today's Date, as explicitly required by the form's instructions ('Current diagnostic required not older than 36 months'). An outdated diagnostic evaluation does not meet BCBSIL's clinical currency requirements and will result in denial of the service request. If the evaluation date exceeds the 36-month threshold, the provider must obtain an updated diagnostic evaluation before resubmitting.
6
Ensures Assessment Completion Date Is Within the Last 30 Days
This check verifies that the Assessment Completion Date in the Baseline & Assessment Info section falls within 30 calendar days prior to the Request Submission Date, as required by the form instructions ('Assessment must be within the last 30 days'). A stale assessment does not accurately reflect the member's current skill levels and behavioral profile, which are essential for appropriate treatment planning. If the assessment date is older than 30 days, the submission will be considered incomplete and must be resubmitted with a current assessment.
7
Ensures Request Submission Date Is at Least Two Weeks Before the Requested Start Date
This check confirms that the form's submission date is at least 14 calendar days before the Assessment Request Start Date or Current Request Start Date, as the form explicitly states 'Submit forms at least two weeks before requested start date.' Submitting too close to or after the requested start date may result in delayed authorization and potential gaps in service delivery for the member. Additionally, the form notes that it must be received within 30 days of the treatment request start date, so the start date must also be validated against this outer boundary.
8
Ensures Cross-State Service Disclosure Is Complete When Applicable
This check verifies that when the 'Services conducted in same state?' question is answered 'No,' the 'If no, what state?' field is populated with a valid U.S. state abbreviation or name. Cross-state service delivery has significant implications for licensure, network participation, and state-specific benefit mandates, all of which affect authorization eligibility. If the 'No' box is checked but the service state field is left blank, the form is incomplete and cannot be evaluated for cross-state compliance.
9
Ensures ABA Supervisor Attestation Is Affirmatively Confirmed
This check verifies that the ABA Supervisor Attestation field is answered 'Yes,' confirming that the supervisor follows BACB supervision guidelines and holds an active license in the state where services are rendered. A 'No' response or a blank field indicates the supervisor does not meet the minimum qualifications required by BCBSIL, which would disqualify the provider from billing for ABA services under this authorization. If the attestation is 'No' or missing, the form must be rejected and the provider must resolve the licensure or compliance issue before resubmitting.
10
Ensures Certification Is Signed by Either the Diagnostic Practitioner or ABA Services Supervisor
This check confirms that exactly one of the two certification checkboxes — 'Diagnostic Practitioner' or 'ABA Services Supervisor' — is selected in the Certification of DX & Treatment Expectation section, and that the corresponding signature and date fields are populated. The certification is a legal attestation of the member's capacity to benefit from ABA services, and an unsigned or uncertified form cannot be processed. If neither or both boxes are checked, or if the signature or date is missing, the form is invalid and must be returned for completion.
11
Ensures Treatment Request Start and End Dates Are Logically Consistent
This check validates that the Assessment Request Start Date precedes the Assessment Request End Date, and that neither date is in the past relative to the submission date. A start date that falls after the end date, or an end date that has already passed, indicates a data entry error that would make the authorization period meaningless. If this logical inconsistency is detected, the form must be returned to the provider for correction of the date range.
12
Ensures ABA Procedure Code Units Are Numeric and Greater Than Zero When Populated
This check verifies that any ABA Procedure Code unit fields that are filled in (97151, 97152, 97153, 97154, 97155, 97156, 97157, 97158) contain positive whole numbers, since 1 unit equals 15 minutes and fractional or zero units are not clinically meaningful. It also checks that at least one procedure code unit field is populated, as a request with no units requested cannot be processed. If a unit value is negative, zero, non-numeric, or if all unit fields are blank, the form must be returned for correction.
13
Ensures Weekly Schedule Session End Times Are After Start Times
This check validates that for every populated ABA session time slot across all days of the week (Monday through Sunday), the session end time is strictly later than the session start time on the same day. An end time equal to or earlier than the start time indicates a data entry error and would result in an invalid or zero-duration session being authorized. If any session time span is found to be illogical, the provider must correct the schedule before the form can be approved.
14
Ensures Fade Plan Hours Are Less Than Current Service Hours
This check verifies that the 'Reduced Hours Per Week' value in the Member's Fade Plan is strictly less than the 'Current Hours Per Week' value, ensuring the fade plan represents an actual reduction in service intensity. A fade plan where the reduced hours equal or exceed the current hours does not constitute a clinically meaningful step-down and may indicate a data entry error. If this inconsistency is detected, the form must be returned to the provider to correct the fade plan details.
15
Ensures Medication Prescriber Information Is Provided When Patient Is Taking Medication
This check confirms that when the 'Patient Taking Medication: Yes' checkbox is selected, both the 'Medication Prescribed By' field and the 'Medication Prescriber Professional Licensure/Credential' field are populated, and that the 'Current Medications and Dosages' field contains at least one entry. Medication information is clinically critical for ABA treatment planning, as certain medications can affect behavior and learning. If the medication checkbox is 'Yes' but the prescriber or medication details are missing, the form is incomplete and must be returned for full disclosure.
16
Ensures Previous ABA Provider History Is Fully Disclosed When Applicable
This check verifies that when 'Yes Other ABA Provider' is selected in the ABA Treatment History section, the 'Initial Date from Other Provider' field is populated with a valid past date, and the prior service intensity (Focused or Comprehensive) and average hours per week are also provided. Incomplete prior treatment history prevents BCBSIL from accurately assessing the member's treatment trajectory and continuity of care. If the 'Yes' box is checked but any of the required prior provider fields are blank, the form must be returned for complete disclosure.
Common Mistakes in Completing BCBSIL ABA Initial Assessment & Clinical Service Request
Many submitters confuse the patient's member ID with the subscriber's ID, or transpose digits when copying from an insurance card. This mismatch causes authorization delays or outright denials because BCBSIL cannot locate the correct policy. Always copy the Subscriber ID and Group number directly from the primary subscriber's insurance card, and double-check each digit carefully. AI-powered form filling tools like Instafill.ai can automatically validate and pre-populate insurance identifiers to prevent transcription errors.
The form explicitly requires that the current diagnosis not be older than 36 months, yet providers frequently attach older evaluation reports without verifying the date. Submitting an expired evaluation will result in the request being denied or returned for additional documentation, causing significant delays in the patient receiving ABA services. Always confirm the Initial Evaluation Date and Most Recent Evaluation Date before submission, and obtain an updated evaluation if the most recent one exceeds the 36-month threshold.
The Baseline & Assessment Info section requires that the current assessment be completed within the last 30 days, but providers often submit assessments that are weeks or months old. This is a common oversight when forms are prepared in advance or when there are scheduling delays between assessment completion and form submission. Verify the Assessment Completion Date against today's date before faxing, and if the assessment is older than 30 days, schedule a new one prior to submitting the request.
The form specifies that 1 unit equals 15 minutes, but providers frequently enter hours instead of units, or miscalculate the total units for the assessment period across codes 97151, 97152, 97153, 97155, 97154, 97158, 97156, and 97157. Entering incorrect unit counts can result in under-authorization or claim denials. Convert all requested time to 15-minute units before entering values (e.g., 1 hour = 4 units), and cross-check the total units against the requested hours per week to ensure consistency.
Providers sometimes check the wrong request type or forget to include the required accompanying documents specific to each type. An Initial Treatment Request requires a Diagnostic Evaluation Report, Provider Baseline and Skills Assessment Instruments, and a Comprehensive Treatment Plan, while a Concurrent Treatment Request requires a Skills Re-Assessment Report and Comprehensive Treatment Plan. Submitting the wrong documents or omitting required attachments will cause the request to be returned or denied. Carefully review the checklist at the top of the Clinical Service Request form before faxing.
The form requires separate NPIs for the Diagnostic Practitioner, the Facility, and the BCBA, and providers frequently leave one or more of these blank or enter the same NPI for multiple entities. An NPI is a 10-digit number, and entering an incorrect or incomplete NPI will prevent BCBSIL from verifying provider credentials, leading to authorization delays. Confirm each provider's individual NPI through the NPPES registry before completing the form, and ensure each field contains the correct, unique 10-digit identifier.
When the patient resides in one state but receives services in another, providers often check 'No' for 'Services conducted in same state?' but then fail to specify the service state in the adjacent field. This omission creates ambiguity about licensure and coverage jurisdiction, which can delay or invalidate the authorization. If services are provided in a different state, always complete the 'If no, what state?' field, and verify that the rendering QHP holds an active license in the state where services are rendered.
Providers frequently describe maladaptive behaviors in general terms (e.g., 'aggression') without specifying frequency, duration, or context, and list treatment goals without measurable criteria or expected mastery dates. BCBSIL reviewers require objective, data-driven information to authorize services, and vague entries often trigger requests for additional clinical information, delaying authorization. For each maladaptive behavior, specify the behavior, its frequency, and the measurement interval (per hour, session, day, or week), and ensure all skill acquisition goals and parent training goals include baseline percentages, current progress data, and expected mastery dates.
The ABA Supervisor Signature, printed name, and clinic name are frequently left blank, or the form is faxed before the supervisor has signed it. Without this certification, the form is considered incomplete and will be returned, restarting the authorization timeline. Ensure the ABA Supervisor reviews and physically signs the form before submission, and confirm the ABA Supervisor Attestation checkbox ('Yes' or 'No') regarding BACB supervision guidelines and active state licensure is also completed.
The form clearly states it must be submitted at least two weeks before the requested start date, and that it must be received within 30 days of the treatment request start date. Providers often submit forms too close to the start date, leaving insufficient time for clinical review, which can result in services beginning without authorization and subsequent claim denials. Build submission deadlines into your scheduling workflow, and use the fax number 877-361-7656 well in advance to ensure timely receipt and processing.
The Member ABA Schedule and Member School and Other Therapy Schedule sections require detailed daily time entries including start times, end times, location (office or home), and lunch/break details for every day services are provided, but providers often leave multiple days blank or enter only partial information. Incomplete schedules make it impossible for reviewers to assess service intensity and potential overlap with school or other therapies, which can delay authorization. Complete every applicable day's schedule in full, including all session time slots and break periods, and indicate the service location for each day.
Providers frequently leave the Treatment Fade/Transition/Discharge Plan section blank or provide only a general statement without specifying the current hours per week, the reduced hours per week, the effective date or duration in months, and measurable criteria for fading. BCBSIL requires a concrete, objective fade plan to demonstrate that treatment is goal-directed and time-limited, and omitting this information can result in denial of the concurrent request. Complete all fade plan fields with specific, measurable criteria, and confirm whether the parent/caregiver is in agreement by checking the appropriate 'Yes' or 'No' box.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out BCBSIL ABA Initial Assessment & Clinical Service Request with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills applied-behavior-analysis-aba-initial-assessment-request-and-clinical-service-request-form-blue-cross-and-blue-shield forms, ensuring each field is accurate.