Yes! You can use AI to fill out Alabama Medicaid Agency ABA Therapy Assessment Form (6/20/19) — Behavior Assessment and Treatment Request (CPT 97151) for Applied Behavioral Analysis for Autism Spectrum Disorder
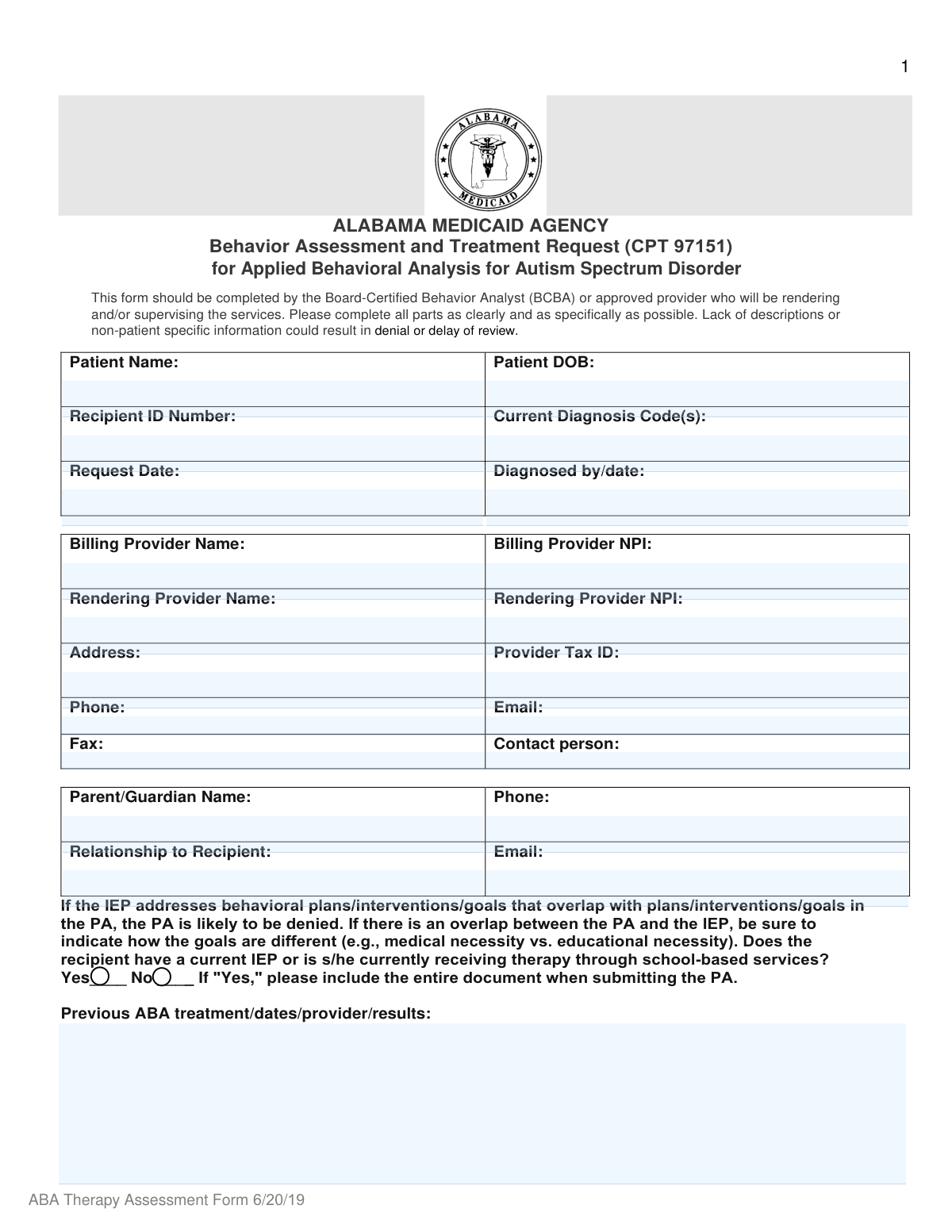
This is an Alabama Medicaid Agency clinical and administrative request form completed by a Board-Certified Behavior Analyst (BCBA) or approved provider to support medical necessity and request authorization for an ABA behavior assessment and treatment planning service billed under CPT 97151. It captures patient identifiers, diagnoses, school-based services/IEP status, clinical history, evaluation findings (e.g., DSM-5 criteria and test scores), targeted behaviors with baselines and measurable goals, and recommended treatment hours/units and coordination/transition plans. The form is important because incomplete or non-patient-specific documentation can lead to delays or denials, and it helps Medicaid reviewers determine whether requested ABA services are appropriate and distinct from educational services. Today, this form can be filled out quickly and accurately using AI-powered services like Instafill.ai, which can also convert non-fillable PDF versions into interactive fillable forms.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out Alabama Medicaid ABA Therapy Assessment (CPT 97151) using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Alabama Medicaid Agency ABA Therapy Assessment Form (6/20/19) — Behavior Assessment and Treatment Request (CPT 97151) for Applied Behavioral Analysis for Autism Spectrum Disorder |
| Number of pages: | 5 |
| Language: | English |
| Categories: | Alabama Medicaid forms, ABA therapy forms, Medicaid therapy forms, Alabama healthcare forms, ABA forms, therapy forms, autism forms |
Instafill Demo: filling out a legal form in seconds
How to Fill Out Alabama Medicaid ABA Therapy Assessment (CPT 97151) Online for Free in 2026
Are you looking to fill out a ALABAMA MEDICAID ABA THERAPY ASSESSMENT (CPT 97151) form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your ALABAMA MEDICAID ABA THERAPY ASSESSMENT (CPT 97151) form in just 37 seconds or less.
Follow these steps to fill out your ALABAMA MEDICAID ABA THERAPY ASSESSMENT (CPT 97151) form online using Instafill.ai:
- 1 Go to Instafill.ai and upload the Alabama Medicaid Agency ABA Therapy Assessment Form (CPT 97151) PDF (or select it from the form library).
- 2 Enter or import patient demographics and identifiers (patient name, DOB, recipient ID) and add current diagnosis code(s) and diagnosing provider/date.
- 3 Complete provider and contact sections (billing/rendering provider names, NPIs, tax ID, address, phone/email/fax, and contact person details).
- 4 Answer the school-based services/IEP question and, if applicable, attach the full IEP and document how ABA medical-necessity goals differ from educational goals to avoid overlap-related denial.
- 5 Use Instafill.ai to draft and refine clinical narrative fields: previous ABA treatment history, co-occurring diagnoses, current symptoms/history, and evaluation findings (DSM-5 criteria, test scores, and natural-setting observations), attaching supporting documentation as needed.
- 6 Fill the Behavioral Targets and Treatment Plan table by listing baseline behaviors/dates, 6-month goals, target mastery dates, long-term goals, and (for subsequent requests) quantified progress percentages for each target.
- 7 Enter recommended treatment hours/sessions and requested CPT codes/units/effective dates for direct patient support and caregiver/parent training, then review for completeness and export/sign/submit per Alabama Medicaid prior authorization instructions.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable Alabama Medicaid ABA Therapy Assessment (CPT 97151) Form?
Speed
Complete your Alabama Medicaid ABA Therapy Assessment (CPT 97151) in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 Alabama Medicaid ABA Therapy Assessment (CPT 97151) form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form Alabama Medicaid ABA Therapy Assessment (CPT 97151)
This form is used to request authorization for an ABA behavior assessment and treatment planning services for a recipient with Autism Spectrum Disorder under Alabama Medicaid. It supports medical necessity by documenting diagnosis, assessment findings, target behaviors, and the proposed treatment plan.
The form should be completed by the Board-Certified Behavior Analyst (BCBA) or an approved provider who will render and/or supervise the ABA services. Incomplete or non-patient-specific information can lead to delays or denial.
You must include the patient’s full name, date of birth, Recipient ID number, and current diagnosis code(s). You should also include the request date and who diagnosed the patient and when.
The form asks for both billing and rendering provider information, including provider names, NPIs, address, Tax ID, phone, email, fax, and a contact person (with title and phone). Make sure the rendering provider information matches the provider who will deliver/supervise services.
Check “Yes” and include the entire IEP document when submitting the prior authorization (PA). The form warns that if IEP goals overlap with PA goals, the PA may be denied, so clearly explain how medical goals differ from educational goals.
State that there is no prior ABA treatment and note “N/A” for dates/provider/results. If there was prior ABA, include dates, provider name, and measurable outcomes or response to treatment.
List any additional diagnoses (behavioral health and medical) that may affect treatment, and summarize relevant symptoms and history. Include information that helps explain current functioning and treatment needs (e.g., sleep issues, seizures, anxiety, aggression, communication deficits).
Briefly summarize DSM-5 criteria support, test scores, and key assessment results, plus observations from natural settings like home and school. Attach supporting documentation or other pertinent findings when available.
For each targeted behavior/skill, document a baseline with a date, a specific measurable 6-month goal, an anticipated mastery date, and long-term goals. For initial requests, baseline data is required; for subsequent requests, provide a new baseline and quantify progress or regression.
If you are requesting continued services, you must report measurable progress (or regression) since the last authorization period, expressed as a percentage toward each goal. Use objective data from treatment records rather than general statements.
Enter recommended hours for Direct Patient Support and the caregiver/parent training frequency (the form notes “1 session per day” for caregiver/parent training). Also specify the setting and number of sessions in a way that matches the units you are requesting on the Prior Authorization.
List the CPT codes requested and the effective units requested to cover 6 months from the effective date, along with the effective date requested. Ensure the units and dates align with the recommended hours/sessions and the 6-month authorization period described on the form.
Provide a brief but specific overview of how ABA will be delivered (e.g., 1:1 home/community hours per week tied to goals), the caregiver training plan, coordination with other providers/school, and a transition plan with anticipated outcomes. Vague descriptions can cause delays or denial.
Yes—AI tools such as Instafill.ai can help auto-fill form fields using the information you provide, reducing manual entry and improving consistency. You should still review all clinical content (baselines, goals, medical necessity statements) for accuracy and compliance.
You can upload the PDF to Instafill.ai, map your patient/provider data, and let the AI populate the fields, then review and export the completed form. If the PDF is flat/non-fillable, Instafill.ai can convert it into an interactive fillable form so you can complete it digitally.
Compliance Alabama Medicaid ABA Therapy Assessment (CPT 97151)
Validation Checks by Instafill.ai
1
Patient Identifiers Required (Name, DOB, Recipient ID)
Validates that Patient Name, Patient DOB, and Recipient ID Number are all present and non-empty. These three fields are the minimum needed to correctly match the request to the Medicaid recipient and avoid misrouting or duplicate records. If any are missing, the submission should be rejected or routed to a manual review queue as incomplete.
2
Date Fields Use Valid Format and Are Real Calendar Dates
Checks that all date fields (Patient DOB, Request Date, Diagnosed by/date, baseline behavior dates, target goal dates, effective dates) follow an accepted format (e.g., MM/DD/YYYY) and represent real dates (no 02/30, no alphabetic characters). Date parsing failures commonly break downstream adjudication and timeline logic. If invalid, the system should flag the specific field and prevent submission until corrected.
3
Chronological Consistency of Key Dates (DOB < Diagnosis/Request/Effective)
Ensures Patient DOB occurs before Diagnosed by/date, Request Date, baseline dates, and effective dates. This prevents impossible timelines (e.g., diagnosis before birth) and supports medical necessity review. If the chronology is inconsistent, the submission should be blocked and the user prompted to correct the offending dates.
4
Request Date Not Unreasonably in the Future or Too Far in the Past
Validates that Request Date is within an acceptable operational window (e.g., not more than X days in the future and not older than Y days, per program rules). Extremely future-dated or stale requests can indicate data entry errors or outdated clinical information. If outside the allowed window, the system should require correction or justification via manual review.
5
Diagnosis Codes Are Valid ICD-10 Format and Not Free-Text Only
Checks that Current Diagnosis Code(s) are provided and match ICD-10 formatting (e.g., letter + 2 digits, optional decimal and additional characters) and are separated consistently if multiple codes are entered. Correct coding is essential for coverage determination and medical necessity review for ASD-related ABA services. If codes are missing or malformed, the request should be flagged and returned for correction.
6
Diagnosed By/Date Completeness and Structure
Validates that the 'Diagnosed by/date' field includes both a clinician identifier (name/credential or provider) and a diagnosis date, not just one or the other. This supports auditability and confirms that the diagnosis is established by an appropriate source. If either component is missing, the submission should be marked incomplete and require update.
7
Provider NPI Format and Check-Digit Validation (Rendering and Billing if present)
Ensures Rendering Provider NPI (and Billing Provider NPI if captured) is exactly 10 digits and passes the NPI Luhn check-digit algorithm. NPI validity is critical for provider identity, enrollment matching, and claims/PA linkage. If the NPI fails format or check-digit validation, the system should block submission and request correction.
8
Provider Tax ID (TIN) Format Validation
Checks that Provider Tax ID is either 9 digits (EIN/SSN-style) and contains only numeric characters (optionally allowing hyphen formatting). A valid TIN is needed for billing entity identification and compliance checks. If invalid, the submission should be rejected or routed for manual verification depending on policy.
9
Phone and Fax Number Format Validation
Validates that Rendering Provider Phone, Contact Person Phone, Parent/Guardian Phone (if present), and Fax contain valid phone numbers (e.g., 10 digits for US numbers, allowing standard punctuation). Correct contact numbers are necessary for follow-up, documentation requests, and coordination of care. If invalid, the system should flag the specific number and require correction before submission.
10
Email Address Syntax Validation (Provider and Parent/Guardian)
Checks that Rendering Provider Email and Parent/Guardian Email (if provided) match standard email syntax (local@domain) and do not contain spaces or invalid characters. Email is often used for time-sensitive requests for additional documentation and status updates. If invalid, the system should prompt correction and optionally allow submission only if an alternate contact method is complete.
11
Address Completeness for Rendering Provider and Parent/Guardian
Validates that the Rendering Provider Address includes at least street, city, state, and ZIP (or that the structured fields are all present if captured separately), and that Parent/Guardian address fields are complete when required. Complete addresses support correspondence, service location verification, and compliance/audit needs. If incomplete, the submission should be flagged as incomplete and prevented from finalization.
12
IEP/School-Based Services Yes/No Must Be Mutually Exclusive and Selected
Ensures exactly one of the IEP/school-based services options is selected (Yes or No), not both and not neither. This question affects medical vs educational overlap review and documentation requirements. If the selection is missing or contradictory, the system should block submission and require a single clear answer.
13
IEP Attachment Requirement When School-Based Services = Yes
If the user indicates 'Yes' for current IEP or school-based services, validates that the entire IEP document is attached (or that an attachment indicator/upload is present). The form explicitly states the IEP must be included and overlap can lead to denial without clarification. If missing, the system should prevent submission or route to a documentation-deficient queue with an explicit missing-attachment error.
14
Behavioral Targets Table Row Completeness and Date Logic
For each behavioral target row that is started (any field filled), validates that all required columns are completed: baseline behaviors and date, 6-month goal, target goal date, and long-term goals. Also checks that the target goal date is after the baseline date and is a valid date. If incomplete or illogical, the system should flag the specific row and require completion/correction.
15
Progress Percentage Validation for Subsequent Requests
Validates that any 'Progress Toward Goals (%)' entries are numeric and within 0–100, and are only required/used for subsequent requests (per form instructions). This prevents nonsensical values (e.g., 150% or text) and supports consistent review of progress/regression. If out of range or non-numeric, the system should block submission or require correction; if an initial request includes progress, it should be flagged for confirmation.
16
Treatment Hours/Sessions and Units Are Numeric, Non-Negative, and Internally Consistent
Checks that recommended direct patient support hours and caregiver/parent training sessions/units are numeric, non-negative, and consistent with the stated frequency (e.g., '1 session per day' should align with the number of sessions/units requested over the 6-month period). This reduces denials due to unit mismatches and prevents accidental over/under-requesting. If inconsistent, the system should flag the discrepancy and require reconciliation before submission.
Common Mistakes in Completing Alabama Medicaid ABA Therapy Assessment (CPT 97151)
People often enter a nickname, misspell the patient name, transpose digits in the Recipient ID, or use a DOB format that doesn’t match what Alabama Medicaid has on file. This can cause the request to be pended for clarification or denied because the recipient cannot be reliably identified. Always copy the patient’s legal name, DOB, and Recipient ID exactly as shown in Medicaid eligibility/ID documentation and double-check for digit swaps. AI-powered form filling tools like Instafill.ai can help by validating formats and flagging mismatches before submission.
A common error is listing a narrative diagnosis (e.g., “autism”) without the actual diagnosis code(s), using DSM codes instead of ICD-10, or omitting co-occurring codes that support medical necessity. This can delay review or lead to denial if the diagnosis does not clearly support ABA under the benefit. Use current ICD-10 codes, include all relevant active diagnoses, and ensure they align with the evaluation findings and history sections. Instafill.ai can help standardize code formatting and reduce omissions by prompting for required code fields.
Submitters frequently leave the “Diagnosed by/date” blank, provide only a year, or enter dates that conflict with the evaluation narrative (e.g., diagnosis date after the request date). Inconsistent timelines raise red flags and often trigger requests for additional documentation. Provide the diagnosing clinician’s name/credentials and the full diagnosis date (MM/DD/YYYY), and ensure the request date matches the actual submission/request timeline. Instafill.ai can enforce date formats and highlight timeline inconsistencies.
It’s very common to put the agency’s NPI in the rendering provider field, list the BCBA as the billing provider, or omit one provider entirely. This can cause authorization to be issued to the wrong entity or be rejected due to credentialing/NPI mismatches. Confirm which entity is the billing provider and which individual/organization is rendering/supervising, and enter the correct names and NPIs in their respective fields. Instafill.ai can reduce these errors by mapping provider profiles to the correct fields and validating NPI length/format.
People often leave out the full mailing address, enter an outdated fax number, or forget the contact person/title/phone—especially when copying from letterhead. Missing contact details can delay review because the agency cannot quickly request clarifications or send determinations. Provide complete, current contact information and ensure the contact person is someone who can respond promptly to Medicaid inquiries. Instafill.ai can auto-fill standardized provider demographics and format phone/fax numbers consistently.
A frequent mistake is checking “No” when the child has an IEP or receives school-based therapy, or checking “Yes” but failing to attach the entire IEP as required. This can lead to denial or delays, especially because the form warns that overlapping goals between the PA and IEP can result in denial. Verify school services status with the caregiver and records, check the correct box, and attach the full IEP when “Yes” is selected. If the PA goals differ from IEP goals, explicitly explain the medical vs. educational necessity distinction; Instafill.ai can prompt for required attachments and consistency checks.
Many submissions list only “ABA previously” without dates, provider name, intensity, or measurable results, or they omit reasons for discharge/regression. Reviewers rely on this section to understand what has been tried and whether the requested plan is justified. Include treatment dates, provider(s), service setting, hours/week, targeted goals, and objective outcomes (progress, plateau, regression, barriers). Instafill.ai can guide structured entry so key elements (dates, provider, results) aren’t forgotten.
A common pitfall is writing a generic summary (or copying boilerplate) without tying findings to DSM-5 criteria, including standardized assessment names/scores, or describing observations at home/school/community. This can result in a “not patient-specific” determination and delay/denial because the form explicitly requires specificity and supporting evidence. Summarize DSM-5 criteria met, list instruments used with scores/interpretation, and describe direct observations in natural settings; attach supporting reports when referenced. Instafill.ai can help by prompting for required components and ensuring the narrative remains patient-specific.
People often leave parts of the chart blank, provide goals like “improve behavior,” omit baseline frequency/duration, or forget the target goal date for mastery. Incomplete or non-measurable targets make it impossible to evaluate medical necessity and progress, which can lead to denial or a request for resubmission. For each target, include an objective baseline with a date, a measurable 6-month goal (frequency/duration/percent independence), a realistic mastery date, and long-term goals. Instafill.ai can enforce completion of all columns and standardize measurable goal formatting.
For reauthorizations, many submitters restate goals but fail to provide the “new baseline” and the percent progress/regression over the previous treatment days. Without quantified progress, reviewers may conclude the treatment is not effective or that documentation is insufficient, causing delays or denial. Include objective data summaries, updated baselines, and percent progress toward each targeted behavior goal, and explain any lack of progress with plan modifications. Instafill.ai can help calculate/format percentages consistently and remind users to update baselines for subsequent requests.
A frequent error is listing recommended hours per week but requesting units that don’t match a 6-month span, omitting CPT codes, or entering an effective date that conflicts with the requested coverage period. Misalignment can cause the authorization to be issued incorrectly or pended for clarification. Reconcile hours/week → units over 6 months, ensure CPT codes requested match the service type (assessment vs. direct vs. caregiver training), and use a clear effective date that matches the PA period. Instafill.ai can help by validating unit math, formatting dates, and flagging inconsistencies between hours, sessions, and units.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out Alabama Medicaid ABA Therapy Assessment (CPT 97151) with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills alabama-medicaid-agency-aba-therapy-assessment-form-62019-behavior-assessment-and-treatment-request-cpt-97151-for forms, ensuring each field is accurate.