Yes! You can use AI to fill out Applied Behavior Analysis Concurrent Service Authorization Request Form (CPT Codes 97153, 97154, 97155, 97156, 97157, 97158, 0373T) – Virginia Department of Medical Assistance Services
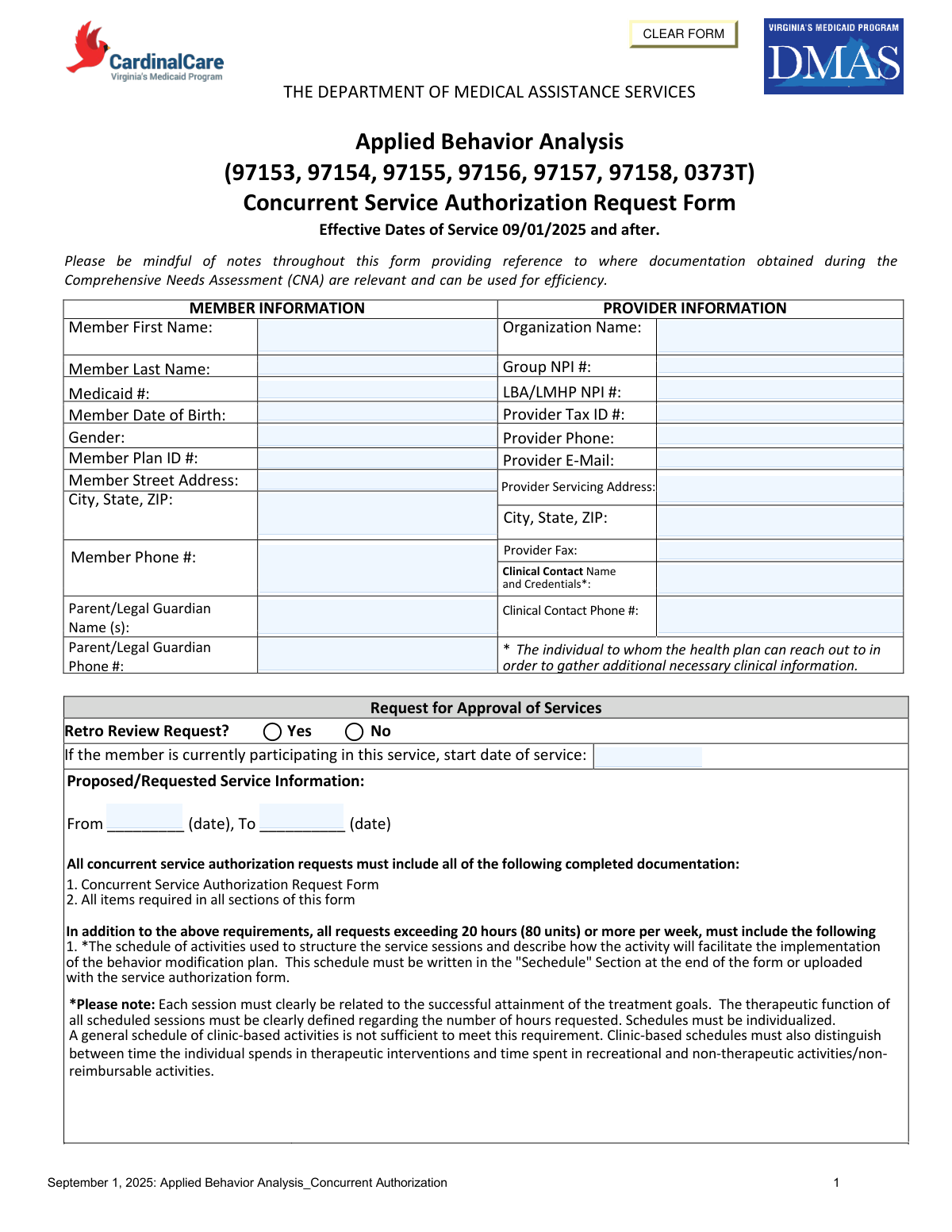
The Applied Behavior Analysis (ABA) Concurrent Service Authorization Request Form is an official Virginia Department of Medical Assistance Services (DMAS) document required for providers to obtain continued Medicaid authorization for ABA therapy services (CPT codes 97153–97158 and 0373T) for members currently enrolled in treatment. The form captures member and provider details, requested service units by CPT code, medication updates, care coordination activities, treatment progress, and recovery and discharge planning to demonstrate ongoing medical necessity. It is effective for dates of service on or after September 1, 2025, and must be accompanied by supporting clinical documentation including an updated Individual Service Plan and treatment progress summary. Today, providers can fill out this detailed form quickly and accurately using AI-powered services like Instafill.ai, which can also convert non-fillable PDF versions into interactive fillable forms.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out ABA Concurrent Authorization Form using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Applied Behavior Analysis Concurrent Service Authorization Request Form (CPT Codes 97153, 97154, 97155, 97156, 97157, 97158, 0373T) – Virginia Department of Medical Assistance Services |
| Number of pages: | 6 |
| Language: | English |
Instafill Demo: filling out a legal form in seconds
How to Fill Out ABA Concurrent Authorization Form Online for Free in 2026
Are you looking to fill out a ABA CONCURRENT AUTHORIZATION FORM form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your ABA CONCURRENT AUTHORIZATION FORM form in just 37 seconds or less.
Follow these steps to fill out your ABA CONCURRENT AUTHORIZATION FORM form online using Instafill.ai:
- 1 Navigate to Instafill.ai and upload the ABA Concurrent Service Authorization Request Form PDF or select it from the available form library to begin filling it out online.
- 2 Complete the Member Information section by entering the member's first and last name, Medicaid ID, date of birth, gender, plan ID, street address, phone number, and parent/legal guardian name and phone number.
- 3 Complete the Provider Information section by entering the organization name, Group NPI, LBA/LMHP NPI, provider tax ID, phone, email, servicing address, fax number, and clinical contact name, credentials, and phone number.
- 4 Fill in the Request for Approval of Services section, indicating whether this is a retro review request, the current service start date if applicable, and the proposed service date range (from/to).
- 5 Enter the requested service details for each applicable CPT code (97153, 97154, 97155, 97156, 97157, 97158, and/or 0373T), including total daily hours/days per week, total weekly hours, total hours requested, total units requested, and any relevant notes; also complete the medication update table with current medications, doses, frequencies, and any changes since the last authorization.
- 6 Complete Sections I through III by documenting care coordination activities and services, attaching or summarizing treatment progress (including ISP goals, graphical data, family involvement, and generalization progress), and filling in the recovery and discharge planning fields including barriers, outreach needs, vision for discharge level of care, and estimated discharge date.
- 7 Review all sections for completeness, attach required supporting documentation (CNA addendum, updated ISP, progress summary, and schedule if 20+ hours/week are requested), then have the supervising LMHP, LMHP-R/S/RP, or LABA sign, print their name, enter their credentials and attestation date, and submit the completed form to the health plan.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable ABA Concurrent Authorization Form Form?
Speed
Complete your ABA Concurrent Authorization Form in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 ABA Concurrent Authorization Form form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form ABA Concurrent Authorization Form
This form is used to request continued (concurrent) authorization for Applied Behavior Analysis (ABA) services through Virginia's Department of Medical Assistance Services (DMAS). It is required when a member is already receiving ABA services and needs ongoing approval for CPT codes 97153, 97154, 97155, 97156, 97157, 97158, and/or 0373T. The form is effective for services dated September 1, 2025 and after.
The form must be completed by the ABA provider organization and signed by a Licensed Mental Health Professional (LMHP, LMHP-R, LMHP-S, LMHP-RP) or a Licensed Behavior Analyst (LABA). The signing clinician is attesting that the member meets medical necessity criteria for the requested ABA services.
All concurrent authorization requests must include the completed form with all sections filled out. Additionally, you must submit the original Comprehensive Needs Assessment (CNA) with an addendum, an updated Individual Service Plan (ISP), and a summary of the youth's treatment progress including graphical data on each goal. Requests exceeding 20 hours (80 units) per week must also include an individualized schedule of activities.
If requesting 20 or more hours (80 or more units) per week, you must include a detailed, individualized schedule of activities that structures the service sessions and explains how each activity facilitates the behavior modification plan. Each session must be clearly linked to treatment goals, and clinic-based schedules must distinguish between therapeutic time and recreational or non-reimbursable activities. A general clinic schedule is not sufficient.
Each CPT code is billed in 15-minute increments, so total units are calculated by multiplying the total hours requested by 4. For example, if you request 240 total hours for CPT 97153, the total units would be 960. Total hours are calculated by multiplying the total weekly hours by the number of weeks in the requested authorization period.
Section II requires a graphical presentation of progress on each ISP goal and objective, an overview of family involvement, a summary of progress toward generalization of skills across multiple settings, and a description of progress toward discharge including plans to reduce services. The ISP must include person-centered treatment goals, objective measures, interventions, dosage, and identified strengths and barriers.
Section III requires you to describe what progress or recovery looks like for the individual, identify barriers to recovery, outline outreach or additional supports needed, describe the anticipated level of care at discharge, and provide a best estimate of the discharge date. Discharge planning should begin at the first contact and reflect the most current understanding of the member's recovery trajectory.
A Retro Review Request is when you are seeking authorization for services that have already been provided rather than for future services. You should select 'Yes' for the Retro Review option if you are requesting approval retroactively for ABA services already delivered to the member.
You must provide the organization name, Group NPI number, LBA/LMHP NPI number, Provider Tax ID, provider phone number, email, fax, and servicing address. You also need to include the clinical contact name with credentials and their phone number, as this is the person the health plan will contact for additional clinical information if needed.
For each medication the member is taking, you must list the medication name, dose, and frequency. If there have been any changes since the last authorization, you must note whether the medication is new, has ended, or has had a change in dose or frequency. Up to four medications can be listed directly on the form.
Section I requires you to list all medical, behavioral, and community services or supports the member has participated in since the last authorization, including the provider contact information, frequency, and any changes (new, ended, or changed in frequency/intensity). You must also describe the care coordination activities that occurred between these services since the last authorization.
Yes, AI-powered services like Instafill.ai can help you accurately auto-fill form fields, saving significant time especially given the complexity and length of this form. These tools can help ensure all required fields are completed correctly and consistently across multiple authorization requests.
You can upload the ABA Concurrent Authorization form to Instafill.ai, where the AI will guide you through each field and auto-fill information based on the member and provider data you provide. This is especially helpful for calculating CPT code units, organizing medication updates, and ensuring all required sections are completed before submission.
If you have a flat, non-fillable PDF version of this form, Instafill.ai can convert it into an interactive fillable form so you can type directly into the fields digitally. This eliminates the need to print and handwrite the form, reducing errors and saving time.
ISP treatment goals must be person-centered, recovery-oriented, and trauma-informed, written in collaboration with the individual using understandable language. Each goal must have objective measures (such as frequency counts or severity ratings), a description of how progress will be tracked, and clearly defined interventions. Goals should leverage individual strengths and address barriers to participation in care.
Compliance ABA Concurrent Authorization Form
Validation Checks by Instafill.ai
1
Member Date of Birth Format and Validity
Validates that the Member Date of Birth is entered in a recognized date format (MM/DD/YYYY) and represents a logically valid date (e.g., not a future date, not more than 120 years in the past). This field is critical for confirming member identity and ensuring the correct individual's record is being processed. If the date is missing, improperly formatted, or logically impossible, the authorization request cannot be accurately matched to the correct Medicaid member record.
2
Medicaid ID Format and Presence
Validates that the Member Medicaid ID is present and conforms to the expected Virginia Medicaid identifier format (typically a numeric string of a defined length). This identifier is the primary key used to link the authorization request to the member's Medicaid account and eligibility record. A missing, malformed, or incorrect Medicaid ID will result in the request being unprocessable or matched to the wrong member, potentially causing claim denials or compliance issues.
3
Group NPI and LBA/LMHP NPI Format Validation
Validates that both the Group NPI and the LBA/LMHP NPI fields contain exactly 10-digit numeric values, consistent with the National Provider Identifier standard established by CMS. NPIs are required to identify the billing and rendering providers and are used to verify provider enrollment and credentialing with the health plan. If either NPI is missing, non-numeric, or not 10 digits, the authorization cannot be properly attributed to a credentialed provider, which may result in denial of the request.
4
Provider Tax ID Format Validation
Validates that the Provider Tax ID is entered in the standard EIN format (XX-XXXXXXX, a 9-digit number with a hyphen after the second digit) or as a 9-digit numeric string. The Tax ID is required for billing and payment processing and must match the provider's enrollment record with DMAS. An incorrectly formatted or missing Tax ID will prevent proper provider identification and may result in payment errors or authorization rejection.
5
Phone Number Format Validation for All Phone Fields
Validates that all phone number fields — Member Phone Number, Parent/Legal Guardian Phone Number, Provider Phone, Clinical Contact Phone Number, and Provider Fax — are entered in a standard 10-digit U.S. phone number format (e.g., (XXX) XXX-XXXX or XXX-XXX-XXXX). Valid contact numbers are essential for the health plan to reach the member, guardian, or clinical contact when additional information is needed to process the authorization. Missing or improperly formatted phone numbers may delay or prevent timely communication and processing of the request.
6
Proposed Service Date Range Logical Consistency
Validates that the Proposed/Requested Service From Date is earlier than or equal to the Proposed/Requested Service To Date, and that both dates fall on or after the effective date of 09/01/2025. The service date range defines the authorization period and must be logically coherent to ensure services are approved for a valid future or concurrent timeframe. If the start date is after the end date, or if dates fall before the policy effective date, the authorization period is invalid and the request must be corrected before processing.
7
CPT Code Total Units Calculation Accuracy
Validates that for each CPT code row (97153, 97154, 97155, 97156, 97157, 97158, 0373T), the Total Units Requested equals the Total Hours multiplied by 4, and that the Total Hours equals the Total Weekly Hours multiplied by the number of weeks in the requested service period. These calculations are mathematically derived fields and must be internally consistent to ensure the correct number of units is authorized and billed. Discrepancies in these calculations may result in over- or under-authorization of services and potential compliance or billing issues.
8
Total Weekly Hours Threshold Triggers Schedule Requirement
Validates that if the combined total weekly hours across all CPT codes exceeds 20 hours (80 units) per week, the Schedule section at the end of the form is completed or a schedule document is uploaded with the request. The form explicitly requires a detailed, individualized schedule of activities for requests exceeding this threshold to justify the intensity of services. If the weekly hours exceed 20 but the schedule section is blank or absent, the request is incomplete and must be returned to the provider for the required documentation.
9
Retro Review Request Indicator Completeness
Validates that the Retro Review Request field has a selection of either 'Yes' or 'No,' and that if 'Yes' is selected, the Service Start Date field is populated with a valid date indicating when the member began participating in the service. The retro review indicator determines whether the authorization covers services already rendered, which requires additional scrutiny and documentation. If the indicator is unselected or if 'Yes' is selected without a corresponding start date, the request is ambiguous and cannot be properly categorized for review.
10
Assessment/Addendum Completion Date Presence and Validity
Validates that the Assessment/Addendum Completion Date is populated with a valid date in MM/DD/YYYY format and that this date is not in the future relative to the submission date. This date documents when the LMHP or LABA completed the required clinical assessment or addendum that supports medical necessity, and it must precede or coincide with the authorization request submission. A missing or future-dated assessment completion date undermines the attestation and may indicate that the required clinical review has not yet occurred.
11
LMHP Printed Name and Credentials Required for Attestation
Validates that both the Printed Name of LMHP (or R/S/RP or LABA) and the Credentials fields are populated and non-empty at the time of submission. The attestation section requires a licensed professional to certify that the member meets medical necessity criteria, and the printed name and credentials are necessary to identify and verify the qualifications of the attesting individual. If either field is blank, the attestation is incomplete and the authorization request lacks the required clinical sign-off, rendering it invalid for processing.
12
Provider Email Address Format Validation
Validates that the Provider E-Mail field contains a properly formatted email address, including an '@' symbol, a domain name, and a valid top-level domain (e.g., .com, .org, .gov). A valid email address is necessary for the health plan to send electronic correspondence, authorization decisions, and requests for additional information to the provider. An improperly formatted or missing email address may result in failed communications and delays in the authorization process.
13
Clinical Contact Name Includes Credentials
Validates that the Clinical Contact Name and Credentials field is not left blank and contains both a name and at least one professional credential designation (e.g., BCBA, LBA, LMHP). The form explicitly notes that this individual is the point of contact for the health plan to gather additional clinical information, and their credentials establish their authority to speak to clinical matters. If this field is missing or contains only a name without credentials, the health plan cannot verify the clinical contact's qualifications, potentially delaying the review process.
14
Care Coordination Activities Description Completeness
Validates that the Care Coordination Activities Description field is not left blank when one or more services or supports are listed in the Care Coordination table in Section I. The form requires providers to describe how they have coordinated with other services since the last authorization, which is a key component of demonstrating integrated, person-centered care. If services are listed but no coordination activities are described, the submission is incomplete and may not meet the documentation requirements for concurrent authorization approval.
15
Discharge Planning Fields Completeness
Validates that all four discharge planning fields in Section III — what progress/recovery looks like, barriers to progress/recovery, necessary outreach and supports, vision for level of care at discharge, and estimated discharge date — are populated with substantive responses and not left blank. Discharge planning documentation is a required component of concurrent authorization requests and demonstrates that the provider is actively working toward the least restrictive level of care. Blank or cursory responses in these fields indicate an incomplete submission and may result in the request being pended or denied pending additional information.
16
Member Full Name Consistency Across Form Pages
Validates that the Member Full Name and Medicaid ID repeated in the headers of pages 2, 3, 4, 5, and 6 are consistent with the Member First Name, Member Last Name, and Medicaid ID entered in the Member Information section on page 1. These repeated fields serve as identifiers to ensure all pages of a multi-page submission belong to the same member's request. Inconsistencies between pages may indicate a data entry error, a mixed-member submission, or a missing page, any of which could result in the authorization being processed for the wrong individual.
Common Mistakes in Completing ABA Concurrent Authorization Form
Providers frequently confuse the Group NPI with the individual LBA/LMHP NPI, entering the same number in both fields or transposing digits. These are distinct identifiers — the Group NPI belongs to the organization, while the LBA/LMHP NPI belongs to the licensed individual clinician. Submitting mismatched or incorrect NPIs will result in authorization denial or processing delays. Always verify both NPIs against your credentialing records before submission, and tools like Instafill.ai can help auto-populate and validate NPI numbers to prevent this error.
The form requires a multi-step calculation: daily hours × days per week = weekly hours, then weekly hours × number of weeks = total hours, then total hours × 4 = total units. Providers commonly make errors at one or more of these steps, especially when rounding partial hours or mixing up the number of weeks in the authorization period. Incorrect unit totals can lead to underpayment, overpayment, or outright denial of the authorization request. Double-check every calculation independently for each CPT code row, and consider using a spreadsheet or an AI-assisted tool like Instafill.ai that can automatically compute these values.
When requesting more than 20 hours (80 units) per week, providers must include a detailed, individualized schedule of activities in the 'Schedule' section at the end of the form or as an uploaded attachment. Many providers overlook this requirement entirely or submit a generic clinic-based schedule that does not distinguish between therapeutic and non-therapeutic/recreational time. This omission is a common cause of authorization denial for high-intensity requests. Carefully review the threshold requirement and ensure the schedule is individualized, session-specific, and clearly tied to treatment goals.
Providers often leave the medication update section blank or fail to note whether a medication is new, ended, or changed in dose or frequency since the last authorization. This section is critical for demonstrating clinical continuity and medical necessity. Reviewers use medication information to assess the member's current clinical status, and incomplete entries can raise questions about the quality of care coordination. For each medication listed, explicitly state whether it is unchanged, new, ended, or modified, even if the change seems minor.
Providers sometimes skip the Retro Review question or mark it incorrectly, not realizing that a retroactive review requires different supporting documentation and has specific submission timelines. Failing to correctly identify a request as retroactive can result in the request being processed under the wrong review pathway, leading to denial. Review the dates of service carefully — if services have already begun or been delivered, the retro review box must be marked 'Yes' and the service start date must be accurately entered.
Section I requires providers to list all medical, behavioral, and community services the member has participated in since the last authorization, including any changes in frequency or intensity. Providers frequently list service names without providing provider contact information or frequency details, or they fail to describe care coordination activities with those services. Incomplete care coordination documentation signals poor clinical oversight and can jeopardize authorization approval. Ensure every service listed includes provider contact info, frequency, and a clear notation of any changes since the last authorization.
Section II requires a detailed, individualized treatment progress summary including graphical data on each goal, family involvement, generalization of skills, and discharge planning progress. Providers often submit templated or boilerplate progress notes that do not reflect the specific member's data, or they omit the graphical presentation of goal progress entirely. Reviewers are trained to identify non-individualized documentation, and such submissions are frequently returned or denied. Each goal must have objective, measurable data presented graphically, and all narrative sections must be specific to the individual member.
The form explicitly cautions against using percentages as objective measures unless the percentage completion is obvious and easily computed. Providers habitually write goals such as '80% accuracy' without defining what constitutes a trial, how trials are counted, or who measures them. This makes progress tracking ambiguous and difficult for reviewers to verify. Instead, use frequency counts of observable behaviors, severity ratings with clearly defined anchors, or standardized validated assessments, and always describe how, how often, and by whom the measure will be tracked.
Section III asks for specific, individualized responses about what recovery looks like, identified barriers, necessary supports, vision for level of care at discharge, and a best-estimate discharge date. Providers frequently leave fields blank, provide one-sentence generic answers, or fail to provide a discharge date estimate because they feel it is too uncertain. However, the form explicitly states that discharge planning should begin at first contact, and vague or missing responses suggest a lack of recovery-oriented planning. Provide thoughtful, individualized answers for each question, even if the discharge date is an estimate with a noted range.
The attestation at the end of the form must be signed by an LMHP, LMHP-R, LMHP-S, LMHP-RP, or LABA — not by a technician, BCBA candidate, or other unlicensed staff. Providers sometimes have the wrong staff member sign, omit credentials entirely, or leave the assessment completion date blank. An invalid signature invalidates the entire authorization request. Verify that the signing clinician holds one of the specifically listed credentials, include their full printed name and credentials, and ensure the assessment or addendum completion date is accurately recorded.
The 'From' and 'To' date fields for the proposed/requested service period are frequently left blank, entered in inconsistent formats (e.g., MM/DD/YY vs. MM/DD/YYYY), or set to dates that fall outside the allowable authorization window or before the effective date of 09/01/2025. Incorrect or missing service dates prevent the health plan from processing the request and may result in gaps in coverage. Always use a consistent date format, confirm the requested period aligns with plan authorization windows, and verify that the start date is not prior to the form's effective date. AI-powered tools like Instafill.ai can automatically validate date formats and flag inconsistencies.
The form has multiple pages, each with fields for 'Member Full Name' and 'Medicaid #' at the top. Providers often complete these fields on the first page but leave them blank on subsequent pages (pages 2–6), assuming the information carries over. If pages become separated during faxing or electronic processing, incomplete continuation pages cannot be matched to the correct member record, causing significant processing delays or loss of documentation. Always fill in the member's full name and Medicaid number on every page of the form before submission.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out ABA Concurrent Authorization Form with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills applied-behavior-analysis-concurrent-service-authorization-request-form-cpt-codes-97153-97154-97155-97156-97157-97158 forms, ensuring each field is accurate.