Yes! You can use AI to fill out Elbow and Forearm Conditions Disability Benefits Questionnaire
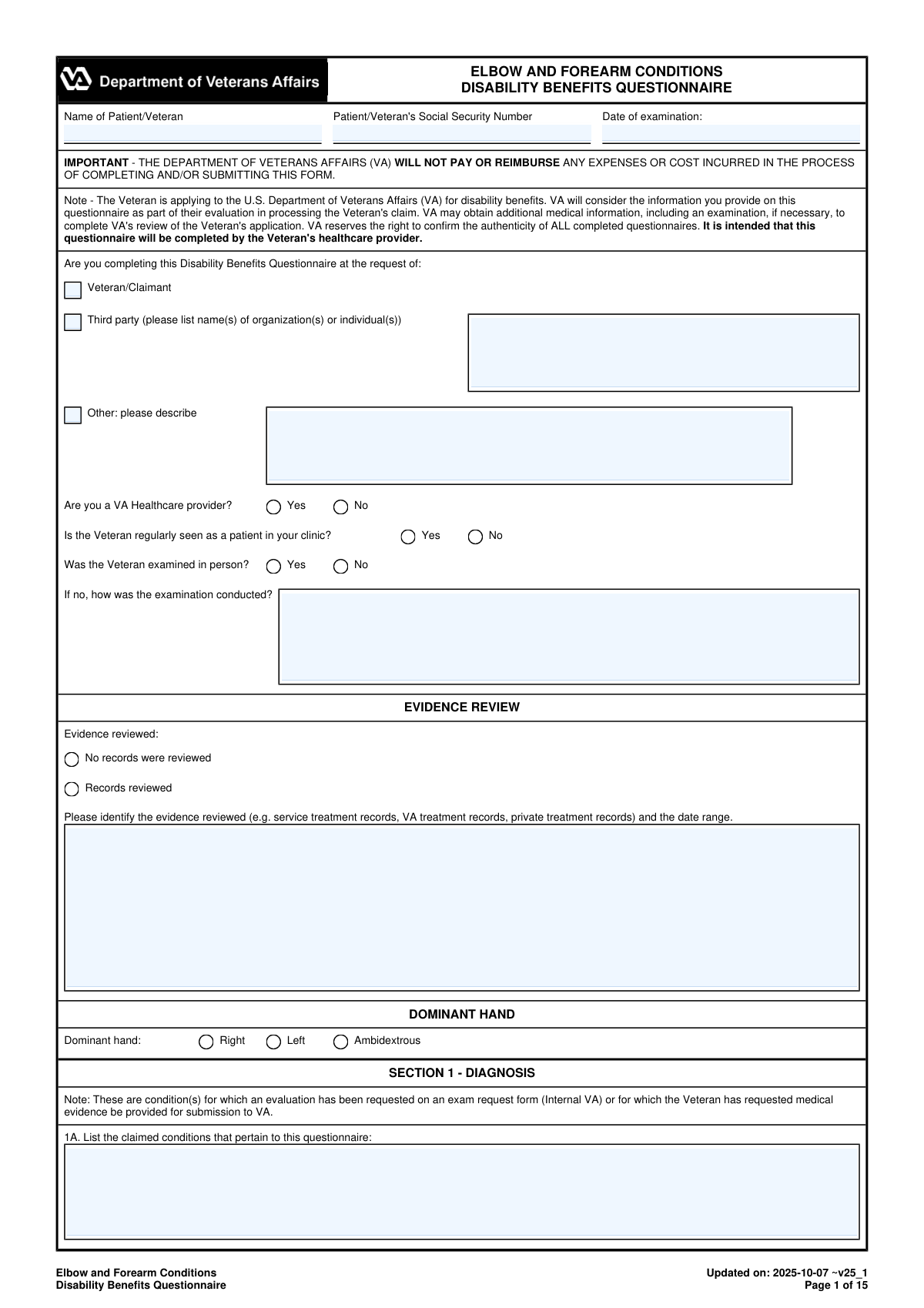
The Elbow and Forearm Conditions DBQ is an official VA medical questionnaire intended to be completed by a qualified healthcare provider to support a Veteran’s disability benefits claim. It captures key clinical findings such as diagnoses, flare-ups, pain, range-of-motion measurements (active/passive, weight-bearing/non-weight-bearing), repetitive-use limitations, ankylosis, other impairments, surgeries, imaging results, and occupational impact. VA uses this standardized format to compare the condition against rating criteria and determine the appropriate disability evaluation. Accurate, complete entries and provider certification/signature are important because VA may verify authenticity and rely on the DBQ as medical evidence in the claim.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out VA DBQ (Elbow and Forearm Conditions) using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Elbow and Forearm Conditions Disability Benefits Questionnaire |
| Number of pages: | 15 |
| Language: | English |
| Categories: | healthcare forms, disability forms, veteran forms, medical disability forms, medical forms, benefit forms |
Instafill Demo: filling out a legal form in seconds
How to Fill Out VA DBQ (Elbow and Forearm Conditions) Online for Free in 2026
Are you looking to fill out a VA DBQ (ELBOW AND FOREARM CONDITIONS) form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your VA DBQ (ELBOW AND FOREARM CONDITIONS) form in just 37 seconds or less.
Follow these steps to fill out your VA DBQ (ELBOW AND FOREARM CONDITIONS) form online using Instafill.ai:
- 1 Enter Veteran/patient identifiers and exam details (name, SSN, date of examination) and indicate who requested the DBQ and whether the exam was in-person.
- 2 Complete the Evidence Review and Dominant Hand sections, listing records reviewed (type and date range) and the Veteran’s dominant hand.
- 3 Document Section 1 (Diagnosis): list claimed conditions, select all applicable elbow/forearm diagnoses, specify side affected, ICD codes, and diagnosis dates, and add clarifying comments if needed.
- 4 Fill Section 2 (Medical History): summarize onset/course, record flare-ups, functional loss, and whether painful motion occurs with flexion/extension or supination/pronation and whether it relates to the claimed condition.
- 5 Record Section 3 (ROM and Functional Limitation): enter right/left active and passive ROM values, note pain (including weight-bearing/non-weight-bearing), crepitus/tenderness, repetitive-use results, and estimates for repeated use over time and flare-ups with supporting rationale.
- 6 Complete remaining clinical sections as applicable (muscle atrophy, ankylosis, other impairments, surgeries, scars/other findings, assistive devices, remaining effective function, and diagnostic testing/imaging results).
- 7 Finish Section 12 (Functional Impact) and Section 13 (Remarks), then complete Section 14 with examiner certification, signature, credentials, NPI/license information, contact details, and date signed before generating the final submission copy.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable VA DBQ (Elbow and Forearm Conditions) Form?
Speed
Complete your VA DBQ (Elbow and Forearm Conditions) in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 VA DBQ (Elbow and Forearm Conditions) form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form VA DBQ (Elbow and Forearm Conditions)
This DBQ documents a Veteran’s elbow and/or forearm diagnoses, symptoms, and functional limitations so VA can evaluate a disability benefits claim. VA uses the information as medical evidence when deciding the claim.
It is intended to be completed by the Veteran’s healthcare provider (clinician). The Veteran can provide history and symptom descriptions, but the medical findings, measurements, and certification should be completed and signed by the examiner.
No. The form states VA will not pay or reimburse any expenses or costs incurred to complete and/or submit the DBQ.
No. The form asks whether the examiner is a VA provider, but non-VA clinicians can complete it as long as they provide the required medical information and credentials.
Not always. If the Veteran was not examined in person, the examiner must indicate “No” and explain how the examination was conducted.
The examiner should indicate whether records were reviewed and identify what was reviewed (e.g., service treatment records, VA records, private records) and the date range. If no records were reviewed, the form allows that option as well.
Dominant hand (right/left/ambidextrous) can affect how VA evaluates functional impact and severity, especially when the condition affects the dominant upper extremity.
The examiner can select that the Veteran does not have a current diagnosis associated with the claimed condition(s) and must explain the findings and reasons in the Remarks section.
If flare-ups are reported, the examiner should record the Veteran’s description, including frequency, duration, characteristics, triggers, relieving factors, and how flare-ups affect function. This information is later used to estimate additional limitation during flare-ups.
The form requests ROM for flexion (145°), extension (0°), forearm supination (85°), and forearm pronation (80°) for each elbow. It also asks for both active and passive ROM and whether pain occurs with motion.
The examiner can mark ROM testing as “Unable to test” or indicate testing cannot be performed, but must provide a clear medical explanation. The form specifically requires an explanation when testing is not done or is medically contraindicated.
Repetitive-use testing measures whether function or ROM decreases after repeated movement (at least three repetitions). The examiner records any additional loss and identifies contributing factors such as pain, weakness, fatigability, lack of endurance, or incoordination.
Yes. The form asks the examiner to estimate ROM during flare-ups and after repeated use over time based on all procurable information, including the Veteran’s statements, records, and medical expertise; if an estimate isn’t feasible, the examiner must explain why.
Degenerative (osteoarthritis) or post-traumatic arthritis must be confirmed by imaging. If arthritis has already been documented by imaging in the past, VA does not require new imaging solely to complete the DBQ, even if symptoms have worsened.
The examiner must sign and date the form and provide printed name/title, specialty, contact information, NPI, medical license number/state, and address. The certification also warns that knowingly submitting false information can result in severe penalties.
Compliance VA DBQ (Elbow and Forearm Conditions)
Validation Checks by Instafill.ai
1
Patient/Veteran Identifiers Present and Properly Formatted
Validate that the Patient/Veteran name, Social Security Number (SSN), and Date of Examination are all present, since they are core identifiers for matching the DBQ to the correct claimant and encounter. SSN should be exactly 9 digits (optionally allowing standard hyphen formatting XXX-XX-XXXX) and must not be all zeros in any group. If any identifier is missing or malformed, the submission should be rejected or routed to manual review because it cannot be reliably associated with the correct Veteran or exam date.
2
Date Fields Use Valid Dates and Logical Chronology
Check that all date fields (Date of examination, Date of diagnosis, surgery dates, diagnostic test dates, Date signed) are valid calendar dates in an accepted format (e.g., YYYY-MM-DD). Enforce logical ordering where applicable: surgery dates and diagnostic test dates should not be after the Date signed, and the Date signed should not precede the Date of examination. If dates are invalid or illogical, flag the record because it undermines medical timeline integrity and can affect rating decisions.
3
Requestor Type Selection and Third-Party Details Completeness
Ensure exactly one requestor type is selected (Veteran/Claimant, Third party, or Other) to avoid ambiguity about who initiated the DBQ. If 'Third party' is selected, require the organization/individual name(s); if 'Other' is selected, require a description. If this validation fails, block submission or require correction because provenance and authorization context are unclear.
4
Provider Status and Examination Modality Consistency
Validate that 'Was the Veteran examined in person?' is answered, and if 'No' is selected, the 'how was the examination conducted' field is completed with a meaningful method (e.g., telehealth/video, records review). Also require an answer for 'Are you a VA Healthcare provider?' and 'Is the Veteran regularly seen as a patient in your clinic?' because these affect credibility and context. If inconsistent or incomplete, route to manual review since the adequacy of the exam may be questioned.
5
Evidence Review Selection Requires Evidence Details When Applicable
Ensure the Evidence reviewed section is internally consistent: if 'Records reviewed' is selected, require the evidence types and a date range; if 'No records were reviewed' is selected, the evidence list/date range should be empty. This prevents contradictory documentation about what sources informed the opinion. If the check fails, prompt correction because evidence basis is required for defensible medical conclusions.
6
Dominant Hand Must Be Selected and Must Be a Single Value
Validate that Dominant hand is selected as exactly one of Right, Left, or Ambidextrous. This is important because dominance can affect functional impact interpretation and rating considerations for upper extremity conditions. If missing or multiple selections occur, prevent submission until corrected.
7
Diagnosis Selection Requires Side, ICD Code Format, and Diagnosis Date
For each checked diagnosis in Section 1B, require a side affected (Right/Left/Both) and validate that the ICD code field matches an expected ICD-10 pattern (e.g., letter + 2 digits + optional decimal and additional characters). Require a Date of diagnosis (or an explicit indication that it is unknown/approximate if your system supports it) to support timeline. If any selected diagnosis lacks these details, flag as incomplete because it impairs downstream adjudication and analytics.
8
Mutual Exclusivity: 'No Current Diagnosis' vs. Any Diagnosis Checked
If 'The Veteran does not have a current diagnosis...' is selected, ensure no other diagnoses are checked in Section 1B and require an explanation in Remarks. Conversely, if any diagnosis is checked, the 'no current diagnosis' option must be unchecked. If violated, block submission because the form contains a direct contradiction about whether a current diagnosis exists.
9
Other Diagnosis Fields Require Specification Text
If 'Other (specify)' or 'Other diagnosis #1/#2' is used, require the free-text diagnosis name and the associated side/ICD/date fields to be completed. This ensures non-standard conditions are still codified and attributable to a limb/side. If missing, fail validation because the diagnosis is not interpretable or rateable.
10
Conditional Narrative Requirements for Yes/No Questions (History, Flare-ups, Functional Loss, Painful Motion)
Enforce that when the Veteran reports flare-ups (2B=Yes), the flare-up description is completed (frequency, duration, precipitating/alleviating factors, severity/functional impairment). When functional loss is reported (2C=Yes), require the Veteran’s description in their own words. When painful motion is reported (2D/2E=Yes), require selection of the specific motion(s), side(s), and whether it relates to claimed conditions; if 'No', require attribution text. If these conditional narratives are missing, flag as incomplete because the DBQ cannot support functional assessment.
11
ROM Numeric Range and Units Validation (Active/Passive/Repeated Use/Flare-ups)
Validate that all ROM endpoints are numeric degrees and within physiologically plausible bounds (e.g., flexion 0–145, extension typically 0 with allowance for hyperextension/contracture within a configured range, supination 0–85, pronation 0–80). Ensure the same joint/side does not contain non-numeric text in degree fields and that 'Same as active ROM' is not accompanied by conflicting numeric entries. If out-of-range or non-numeric values are found, reject or flag because they indicate data entry errors that can materially change disability evaluation.
12
ROM Testing Feasibility Requires Explanation When Not Performed
If 'Can testing be performed?' is marked 'No' for either elbow, require an explanation (e.g., severe pain, risk of injury, contraindication). Similarly, if ROM is marked 'Unable to test' or 'Not indicated', require the corresponding explanation field to be completed. If missing, fail validation because VA guidance requires justification for omitted measurements.
13
Repetitive-Use Logic: Additional ROM Values Only When Additional Loss = Yes
In Section 3B, if 'Is there additional loss of function, or range of motion, after three repetitions?' is 'Yes', require the post-test ROM endpoints and at least one contributing factor (pain, fatigability, weakness, etc.). If it is 'No', ensure post-test ROM fields are blank to avoid contradictory data. If inconsistent, flag because it creates ambiguity about whether repetitive testing changed function.
14
Repeated Use Over Time / Flare-up Estimation Requires Evidence Citation or Feasibility Rationale
When procured evidence suggests significant limitation with repeated use over time or flare-ups (3C/3D limitation question = Yes), require estimated ROM values in degrees or a specific explanation of why an estimate cannot be provided, plus case-specific evidence citation/discussion. This is critical for compliance with VA expectations on functional loss estimation beyond observed testing. If missing, route to manual review or block submission because the report may be deemed inadequate.
15
Muscle Atrophy Measurements and Causation Completeness
If muscle atrophy is marked 'Yes' (4A), require whether it is due to the claimed condition (4B) and, if due, require location and circumference measurements for normal and atrophied sides in centimeters. Validate that circumferences are positive numbers and that the atrophied side is not larger than the normal side unless an explanation is provided. If incomplete or illogical, flag because atrophy findings affect severity assessment and must be measurable and attributable.
16
Examiner Certification Block Completeness and Identifier Formatting (NPI/License/Phone)
Require completion of examiner signature, printed name/title, specialty, date signed, contact phone/fax, NPI, medical license number/state, and address. Validate NPI as a 10-digit numeric identifier (with optional checksum validation if supported) and validate phone/fax numbers using a consistent format (e.g., 10 digits with optional separators and extension). If any required credential fields are missing or malformed, reject or hold because VA may not accept an unsigned/uncredentialed DBQ and authenticity cannot be confirmed.
Common Mistakes in Completing VA DBQ (Elbow and Forearm Conditions)
People often leave the header fields blank or enter identifiers that don’t match the Veteran’s claim file (e.g., nickname, transposed SSN digits, or missing date of exam). This can delay processing because VA staff may be unable to confidently associate the DBQ with the correct claimant or encounter. Always enter the Veteran’s legal name as used on VA records, verify the SSN digit-by-digit, and include the actual examination date (not the date the form was signed).
A common error is checking multiple requestor options or selecting “Third party” without listing the organization/individual. This creates ambiguity about the purpose and chain of custody of the document, which can trigger follow-up requests or authenticity checks. Choose exactly one requestor category and, if “Third party” or “Other” is selected, provide the full name and a brief description of the request context.
Clinicians sometimes mark “Was the Veteran examined in person? No” but fail to describe how the exam was conducted, or they mark “Yes” while also completing the “If no, how was the examination conducted?” line. These inconsistencies can undermine credibility and may cause VA to order a new C&P exam. Ensure the in-person/telehealth status is consistent and, if not in person, document the method (video/phone/records review), limitations, and what objective measures could not be obtained.
It’s very common to check “Records reviewed” but not identify which records (STRs, VA, private) or the date range. VA relies on this to understand what information informed the medical conclusions and whether key evidence was considered. List the specific sources and approximate date ranges (e.g., “VA treatment records 2018–2025; private ortho notes 2022–2024; imaging 2023-06-10”).
Dominance is frequently skipped or guessed, especially when symptoms are bilateral, but it affects rating considerations and functional impact interpretation. An incorrect dominance entry can lead to an inaccurate evaluation of severity and occupational limitations. Ask the Veteran directly which hand is dominant for writing/most tasks and select Right/Left/Ambidextrous accordingly.
A frequent mistake is selecting conditions (e.g., lateral epicondylitis) but leaving side affected, ICD code, and date of diagnosis blank, or simultaneously checking “no current diagnosis” while also listing diagnoses. This creates internal conflicts and can cause VA to discount the DBQ or request clarification. For each selected diagnosis, complete side (Right/Left/Both), provide the ICD code if known, and include an approximate diagnosis date; if there is truly no diagnosis, check that box and explain clearly in Remarks.
Many submissions mark that flare-ups or functional loss exist but provide no description of frequency, duration, triggers, alleviating factors, and functional impact in the Veteran’s own words. Without these specifics, VA cannot properly evaluate severity over time and may schedule another exam. When “Yes” is selected, document a structured narrative (how often, how long, what activities worsen it, what helps, and what the Veteran cannot do during flare-ups/repeated use).
ROM fields are often left blank, entered as ranges (e.g., “0–120”) instead of endpoints, or recorded in a way that conflicts with normal anatomy (e.g., extension greater than 0 without explanation, or pronation/supination swapped). These errors can invalidate the usefulness of the ROM section and lead to rework. Record numeric endpoints in degrees for flexion, extension, supination, and pronation for each elbow, and double-check that values are plausible and labeled correctly.
Examiners frequently document only active ROM and omit passive ROM and the pain evidence checkboxes, or they skip contralateral testing without stating a medical contraindication. VA guidance expects documentation of pain on active/passive and weight-bearing/non-weight-bearing when feasible, and missing elements often trigger an addendum request. Complete both active and passive ROM sections, indicate where pain is present, and if any testing cannot be performed, provide a specific medical reason (e.g., risk of injury, severe pain).
A very common issue is leaving the “after three repetitions” ROM blank or failing to provide estimated ROM loss for repeated use over time and flare-ups when the Veteran reports limitations. VA often requires an estimate based on procurable information, and “cannot determine” without a case-specific rationale can be rejected. If testing is not possible, explain why; if not observed during flare-up/repeated use, provide a reasoned estimate using the Veteran’s statements, records, and clinical judgment, and cite the evidence used.
People often check that surgery occurred but omit the date/type and residuals, or they diagnose degenerative/post-traumatic arthritis without documenting imaging evidence. This can lead to VA discounting the diagnosis or requesting imaging confirmation. For any surgery, provide the procedure type, date (even approximate), and current residuals; for arthritis diagnoses, document the imaging modality/date and summarize the findings that confirm it.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out VA DBQ (Elbow and Forearm Conditions) with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills elbow-and-forearm-conditions-disability-benefits-q forms, ensuring each field is accurate.