Yes! You can use AI to fill out Form CH-006: PA-BH-Res-PCS, Oregon Behavioral Health Support Program Plan of Care Authorization (Plan of Care Request for Behavioral Health Residential or Personal Care Services)
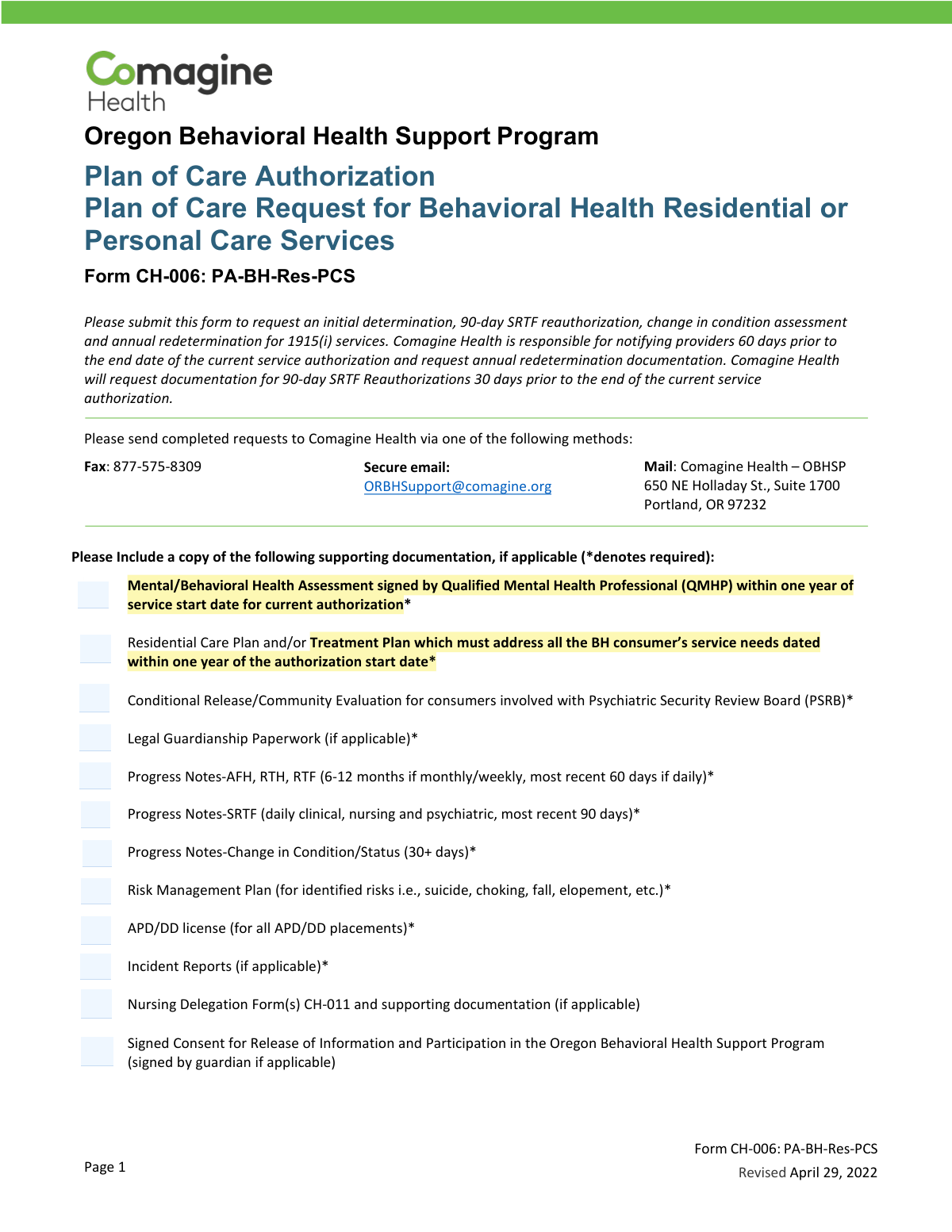
Form CH-006 (PA-BH-Res-PCS) is an Oregon Behavioral Health Support Program plan-of-care authorization request used to obtain approval for 1915(i) behavioral health residential or personal care services. Providers and Community Mental Health Programs (CMHPs) use it to request an initial authorization, a 90-day SRTF reauthorization, a change-in-condition assessment, or an annual redetermination. The form captures member details, legal/guardian status, provider information, level of care, procedure codes/modifiers, and requested service dates/units. Submitting the required supporting clinical documentation is essential for Comagine Health to review and issue or continue service authorization.
Our AI automatically handles information lookup, data retrieval, formatting, and form filling.
It takes less than a minute to fill out CH-006 (PA-BH-Res-PCS) using our AI form filling.
Securely upload your data. Information is encrypted in transit and deleted immediately after the form is filled out.
Form specifications
| Form name: | Form CH-006: PA-BH-Res-PCS, Oregon Behavioral Health Support Program Plan of Care Authorization (Plan of Care Request for Behavioral Health Residential or Personal Care Services) |
| Number of pages: | 3 |
| Filled form examples: | Form CH-006 (PA-BH-Res-PCS) Examples |
| Language: | English |
| Categories: | legal service forms, CAR forms, health care forms, behavioral health forms, authorization forms, service authorization forms, L.A. Care forms |
Instafill Demo: filling out a legal form in seconds
How to Fill Out CH-006 (PA-BH-Res-PCS) Online for Free in 2026
Are you looking to fill out a CH-006 (PA-BH-RES-PCS) form online quickly and accurately? Instafill.ai offers the #1 AI-powered PDF filling software of 2026, allowing you to complete your CH-006 (PA-BH-RES-PCS) form in just 37 seconds or less.
Follow these steps to fill out your CH-006 (PA-BH-RES-PCS) form online using Instafill.ai:
- 1 Select the request type (Initial Request, Annual Redetermination, 90-day SRTF Reauthorization, or Change in Condition) and gather the required supporting documents (e.g., QMHP assessment, care/treatment plan, progress notes, releases, guardianship paperwork if applicable).
- 2 Enter Individual/Member Information: name, date of birth, primary ICD-10 diagnosis code, Medicaid ID, and legal status (Voluntary, Civil Commitment, PSRB, etc.).
- 3 Complete Guardian Information if applicable: guardian name, relationship, address, phone, and email.
- 4 Fill in Request Information: date of admission (if applicable), county of responsibility, CCO, and the Referring Provider’s name, MCD number, phone, email, and fax.
- 5 Complete Rendering Provider details: provider name, MCD number, phone, email, and fax.
- 6 Select the Level of Care and Procedure Code, choose all applicable modifiers, and enter the number of units requested and dates of service (from/to).
- 7 Confirm the individual/guardian is aware of the referral, obtain required signatures (CMHP representative and provider/staff submitting), then submit the completed form and attachments to Comagine Health via fax, secure email, or mail.
Our AI-powered system ensures each field is filled out correctly, reducing errors and saving you time.
Why Choose Instafill.ai for Your Fillable CH-006 (PA-BH-Res-PCS) Form?
Speed
Complete your CH-006 (PA-BH-Res-PCS) in as little as 37 seconds.
Up-to-Date
Always use the latest 2026 CH-006 (PA-BH-Res-PCS) form version.
Cost-effective
No need to hire expensive lawyers.
Accuracy
Our AI performs 10 compliance checks to ensure your form is error-free.
Security
Your personal information is protected with bank-level encryption.
Frequently Asked Questions About Form CH-006 (PA-BH-Res-PCS)
Form CH-006 is used to request authorization for Oregon Behavioral Health Support Program 1915(i) services for Behavioral Health Residential or Personal Care Services. It supports initial determinations, 90-day SRTF reauthorizations, change-in-condition assessments, and annual redeterminations.
The form is typically completed and submitted by the provider or staff requesting services, along with the Community Mental Health Program (CMHP) representative. Both the CMHP representative and the provider/staff submitting the form must sign.
You can submit the completed form to Comagine Health by fax (877-575-8309), secure email ([email protected]), or mail to Comagine Health – OBHSP, 650 NE Holladay St., Suite 1700, Portland, OR 97232.
Required items (marked with an asterisk on the form) generally include a QMHP-signed Mental/Behavioral Health Assessment within one year, a Residential Care Plan/Treatment Plan within one year, and applicable progress notes. Other required documents may include PSRB Conditional Release/Community Evaluation and legal guardianship paperwork when applicable.
For AFH/RTH/RTF, submit 6–12 months if notes are monthly/weekly, or the most recent 60 days if notes are daily. For SRTF, submit daily clinical, nursing, and psychiatric notes for the most recent 90 days; for change in condition/status, provide 30+ days of notes.
Annual redetermination referrals are accepted 60 days prior to the end of the current plan of care. Comagine Health also notifies providers 60 days before the current authorization end date and requests annual redetermination documentation.
A 90-day SRTF reauthorization referral is accepted 30 days prior to the end of the current plan of care. Comagine Health will request documentation for these reauthorizations 30 days before the current authorization ends.
A Change in Condition request is used when there has been a change in the individual’s status that affects service needs. The form indicates these referrals are accepted after 30+ days of change in status, and you should include 30+ days of related progress notes.
You must provide the individual’s name, date of birth, primary ICD-10 diagnosis code, Medicaid ID (prime number), and legal status. If the person has a guardian, you must also complete the guardian information section.
Select the one option that matches the individual’s current legal status: Voluntary, Voluntary by Guardian, Civil Commitment, PSRB, 370, or Aid and Assist. If the person is under guardianship or PSRB involvement, include the required supporting legal documents.
Both sections request the provider name, MCD number, phone number, email address, and fax number. The rendering provider is the provider delivering the services, while the referring provider is the one initiating the referral.
Choose one Level of Care option that matches the placement (e.g., AFH, RTH, SRTF, RTF, APD RCF, ALF, DD AFH, DD Group Home, Independent Living, etc.). Then select the appropriate procedure code (T1020, S5140, S5141, or N/A for Independent Living) and any applicable modifiers (HK, HE, TG, HW).
Enter the requested service span in the Dates of Service “From” and “To” fields using MM/DD/YYYY. If applicable, also provide the Date of Admission to the Residential Program in MM/DD/YYYY.
The form asks whether the individual/guardian is aware the referral is being submitted on their behalf, so you should answer Yes or No accurately. A signed Consent for Release of Information and Participation in the Oregon Behavioral Health Support Program is listed as supporting documentation (signed by the guardian if applicable).
If the individual is involved with PSRB, include the Conditional Release/Community Evaluation. For APD/DD placements, include the APD/DD license; if there are identified risks (e.g., suicide, choking, falls, elopement), include a Risk Management Plan, and include incident reports and nursing delegation forms (CH-011) if applicable.
Compliance CH-006 (PA-BH-Res-PCS)
Validation Checks by Instafill.ai
1
Member name fields present and non-placeholder
Validates that the Individual/Member Last Name and First Name are both provided and contain alphabetic characters (allowing common punctuation like hyphens and apostrophes). This prevents submissions that cannot be matched to eligibility/clinical records or that contain placeholders (e.g., 'N/A', 'Unknown'). If validation fails, the form should be rejected and routed back for correction because downstream authorization and record matching will be unreliable.
2
Date of Birth format and plausibility
Checks that Date of Birth is present, follows a valid date format (MM/DD/YYYY), and represents a plausible date (not in the future and not unreasonably old, e.g., >120 years). This is important for identity verification and for age-dependent level-of-care options (e.g., TAY programs). If it fails, block submission and request correction to avoid misidentification and incorrect service placement.
3
Primary ICD-10 diagnosis code format validation
Ensures the Primary ICD-10 Diagnosis Code is provided and matches ICD-10 formatting rules (e.g., one letter followed by 2 digits, optional decimal and additional characters such as F32.1). Accurate diagnosis coding is required for medical necessity review and correct authorization categorization. If invalid or missing, flag as incomplete and prevent submission until corrected.
4
Medicaid ID (prime number) required and format/length check
Validates that the Medicaid ID is present and conforms to expected character set and length rules used by the program (e.g., numeric-only if required, or alphanumeric if allowed, with no spaces). This is critical for eligibility verification and linking the request to the correct member record. If validation fails, the request should not proceed because eligibility and prior authorizations cannot be reliably retrieved.
5
Legal status selection is exactly one and consistent
Checks that exactly one Legal Status option is selected (Voluntary, Voluntary by Guardian, Civil Commitment, PSRB, 370 Aid and Assist). This matters because legal status can drive required documentation (e.g., PSRB conditional release/community evaluation) and care coordination requirements. If multiple or none are selected, the submission should be rejected as ambiguous and returned for clarification.
6
Guardian information required when legal status implies guardian involvement
If 'Voluntary by Guardian' is selected or guardian involvement is otherwise indicated, validates that Legal Guardian Name, Relationship, Address, Phone, and Email are completed. This ensures legal authority and contactability for consent and participation requirements. If missing, the form should be flagged as incomplete and held until guardian details are provided.
7
Guardian contact format validation (phone and email)
Validates that the Legal Guardian Phone is a valid US phone number (10 digits with optional punctuation) and that the Legal Guardian Email Address matches standard email syntax. Correct contact information is essential for consent, notifications, and coordination. If invalid, the system should prompt for correction and prevent submission to avoid failed outreach and compliance issues.
8
Request type selection is exactly one and drives timing rules
Ensures exactly one request type is selected (Initial Request, Annual Redetermination, 90-day SRTF Reauthorization, Change in Condition Request). The request type determines what documentation is expected and whether the request is timely relative to the current authorization end date. If multiple/none are selected, reject submission; if selected but timing rules cannot be evaluated due to missing dates, flag for follow-up.
9
Admission date required/conditional and valid date
Validates that 'Date of Admission to Residential Program' is provided when applicable (e.g., Initial Request or when a residential placement is indicated) and that it is a valid MM/DD/YYYY date not in the future. Admission date supports eligibility for the requested level of care and aligns the start of services. If missing or invalid when required, the request should be returned for completion.
10
County of Responsibility and CCO required fields
Checks that County of Responsibility and Coordinated Care Organization (CCO) are populated with non-empty values. These fields are necessary for jurisdictional routing, payer coordination, and correct program oversight. If either is missing, the submission should be blocked because the request cannot be properly assigned or processed.
11
Referring provider identifiers and contact information completeness
Validates that Referring Provider Name and MCD Number are present, and at least one reliable contact method is provided (phone or email; fax optional but validated if present). This ensures reviewers can obtain clarifications and verify referral details. If missing or incomplete, the form should be flagged and returned because the referral source cannot be authenticated or contacted.
12
Rendering provider identifiers and contact information completeness
Ensures Rendering Provider Name and MCD Number are present, and at least one contact method (phone or email) is provided; validates formats for phone/email/fax if entered. Rendering provider details are required to issue an authorization to the correct entity and avoid payment/claim mismatches. If validation fails, prevent submission to avoid authorizing services to an unidentifiable provider.
13
Level of Care selection is exactly one and compatible with request type
Checks that exactly one Level of Care is selected (e.g., AFH, RTH, SRTF, DD AFH, DD Group Home, APD RCF, APD ALF, TAY RTH, TAY RTF, APD AFH, Independent Living, RTF). Also validates compatibility rules where applicable (e.g., 90-day reauthorization is specific to SRTF, so Level of Care should be SRTF for that request type). If inconsistent, the system should reject or require confirmation/correction to prevent incorrect authorization pathways.
14
Procedure code required and consistent with Level of Care (including N/A rule)
Validates that a Procedure Code is selected (T1020, S5140, S5141, or N/A) and that 'N/A (Independent Living)' is only used when Level of Care is Independent Living. Procedure codes drive billing and authorization units, so mismatches can cause claim denials and incorrect service tracking. If inconsistent, block submission and prompt the user to select the correct code.
15
Modifiers selection validation (allowed set and duplicates)
Ensures all selected modifiers are within the allowed set (HK, HE, TG, HW) and that no modifier is selected more than once. Modifiers affect service interpretation and reimbursement, so invalid entries can lead to incorrect authorizations and billing errors. If invalid modifiers are detected, reject submission and require correction.
16
Units requested is numeric, positive, and reasonable for date span
Validates that Number of Units Requested is provided, numeric (integer or program-allowed decimal), greater than zero, and within a reasonable maximum based on the Dates of Service duration and typical unit definitions. This prevents over-authorization, under-authorization, and data entry errors (e.g., extra zeros). If it fails, the system should block submission and request corrected units or justification.
17
Dates of Service range validation (format, order, and alignment)
Checks that both 'From' and 'To' Dates of Service are present, valid MM/DD/YYYY dates, and that the 'To' date is on or after the 'From' date. It should also validate that the service dates are not unreasonably far in the past/future per program rules and, when applicable, align with admission date (e.g., service start not before admission for residential placement). If invalid, reject submission to prevent authorizations with impossible or conflicting service periods.
18
Member/guardian awareness question required and consistent with guardian status
Validates that the Yes/No question 'Is the individual/guardian aware this referral is being submitted on their behalf?' is answered. If a guardian is indicated, the logic should ensure the response reflects that either the individual or guardian is aware, and flag 'No' for compliance review. If unanswered, block submission; if 'No', allow submission only with an alert/workflow requiring follow-up documentation or explanation.
19
Signature blocks completeness and date validity
Ensures both signature sections (CMHP Representative and Provider/Staff Submitting Form) include a signature indicator, printed Name and Title, and a Date, with dates in valid format and not in the future. Signatures attest to review and recommendation, which is essential for authorization integrity and audit compliance. If any element is missing or invalid, the form should be rejected as non-compliant.
Common Mistakes in Completing CH-006 (PA-BH-Res-PCS)
People often submit the CH-006 without the required attachments (especially the QMHP-signed assessment and the Residential Care Plan/Treatment Plan) or they attach versions older than the “within one year of authorization start date” requirement. This happens because the checklist is long and the date rules vary by document type (e.g., SRTF notes most recent 90 days vs. AFH/RTH/RTF notes 6–12 months or most recent 60 days if daily). Missing/expired documentation commonly leads to delays, requests for more information, or denial. Avoid this by using the form’s checklist as a packet cover sheet and verifying each document’s signature and date window before sending.
Applicants frequently check the wrong box under “This request is for,” especially confusing Annual Redetermination with 90-day SRTF Reauthorization or using Change in Condition when the change has not met the 30+ day threshold. The consequences include the request being processed under the wrong timeline, missing the correct documentation set, or being rejected as premature. This mistake happens because the acceptance windows (60 days prior, 30 days prior, after 30+ days) are easy to overlook. Avoid it by confirming the current authorization end date and matching it to the correct submission window before selecting the request type.
A common error is entering an incomplete Medicaid ID (or using a non-prime/incorrect number), transposing digits in the date of birth, or listing a non-specific/incorrect ICD-10 code. These mistakes happen due to copying from older records or mixing identifiers from different systems. The result is delayed matching to the correct member record, requests for clarification, or processing under the wrong diagnosis. Avoid this by copying directly from the member’s current eligibility/registration record and double-checking the ICD-10 format and accuracy.
People often skip the Legal Status selection or choose a status (e.g., PSRB, Civil Commitment, Voluntary by Guardian) that doesn’t align with the documentation provided. This can trigger follow-up requests, especially when PSRB is selected but the Conditional Release/Community Evaluation is not included, or when guardianship is indicated but paperwork is missing. The confusion usually comes from not knowing which legal category applies at the time of submission. Avoid this by confirming the current legal status in the chart/court documents and attaching the corresponding required paperwork.
A frequent issue is filling in guardian fields without attaching legal guardianship documentation, or selecting “Voluntary by Guardian” while leaving guardian name/relationship/contact blank. This happens when staff assume guardianship is “on file” elsewhere or misunderstand when it is required. Consequences include delays, inability to confirm consent, and potential compliance issues for releases and participation consent. Avoid this by completing all guardian fields whenever a guardian is involved and always including the guardianship paperwork and guardian-signed consent when applicable.
Submitters sometimes select a level of care that doesn’t match the placement (e.g., checking RTF instead of SRTF, or selecting APD RCF/ALF when the setting is a DD Group Home). This often occurs because acronyms are similar and some settings overlap in everyday language. The consequence can be incorrect authorization parameters, mismatched procedure codes, or a request for resubmission. Avoid this by verifying the licensed setting type and program category (APD vs DD vs TAY) before checking the box.
Common mistakes include choosing the wrong procedure code, forgetting required modifiers, selecting modifiers that don’t apply, or marking “N/A (Independent Living)” while also requesting a residential level of care. These errors happen because coding rules are easy to mix up across settings and staff may reuse old templates. Consequences include claim/authorization mismatches, rework, and processing delays. Avoid this by confirming the correct code/modifier combination for the selected level of care and ensuring the selection is internally consistent across the form.
People often enter “Number of Units Requested (over full duration)” that doesn’t match the From/To dates, or they leave dates blank, use the wrong format, or request dates outside the allowable authorization period. This happens when the unit calculation is done separately or when the admission date is confused with the authorization start date. The result is follow-up questions, partial approvals, or denial for incorrect service periods. Avoid this by calculating units based on the exact From/To range and using MM/DD/YYYY consistently for admission and service dates.
For requests tied to residential admission, submitters sometimes omit the “Date of Admission to Residential Program” or enter it in a non-MM/DD/YYYY format. This occurs because the field is labeled “if applicable,” leading people to assume it’s optional even when it’s needed to establish timing for an initial request or placement. Missing/incorrect admission dates can delay review and create confusion about eligibility and service start. Avoid this by including the admission date whenever the member is in (or entering) a residential program and formatting it exactly as MM/DD/YYYY.
A common problem is leaving the MCD number blank, providing a facility name without the correct provider identifier, or entering the rendering provider details in the referring provider section (and vice versa). This happens when multiple organizations are involved and staff are unsure who should be listed where. Consequences include delays in contacting the right party, misrouted determinations, and authorization issued to the wrong provider. Avoid this by confirming which entity is the referrer vs renderer and ensuring each section includes the correct MCD number, phone, email, and fax.
Submissions are often missing one of the two required signature lines (CMHP Representative and Provider/Staff Submitting Form), or they include a signature without printed name/title and date. This happens when forms are routed between teams and one party assumes the other will sign later. The consequence is an incomplete request that cannot be processed until corrected. Avoid this by verifying both signature blocks are fully completed (signature, name and title, and date) before faxing/emailing/mailing the packet.
Saved over 80 hours a year
“I was never sure if my IRS forms like W-9 were filled correctly. Now, I can complete the forms accurately without any external help.”
Kevin Martin Green
Your data stays secure with advanced protection from Instafill and our subprocessors



Robust compliance program
Transparent business model
You’re not the product. You always know where your data is and what it is processed for.
ISO 27001, HIPAA, and GDPR
Our subprocesses adhere to multiple compliance standards, including but not limited to ISO 27001, HIPAA, and GDPR.
Security & privacy by design
We consider security and privacy from the initial design phase of any new service or functionality. It’s not an afterthought, it’s built-in, including support for two-factor authentication (2FA) to further protect your account.
Fill out CH-006 (PA-BH-Res-PCS) with Instafill.ai
Worried about filling PDFs wrong? Instafill securely fills form-ch-006-pa-bh-res-pcs-oregon-behavioral-health forms, ensuring each field is accurate.